by Sheila Coogan, MD, Dianna Milewicz, MD and Hariyadarshi Pannu, PhD


Varicose veins are one of the most common medical conditions in the western world, with 23% (about one-fourth) of adults in the United States affected with disease.1 Interestingly, this is one of the vascular diseases that is significantly more common in women than men, with twice as many women affected compared to men. Recent data shows that in the United States, varicose veins affect more than 22 million women and 11 million men between the ages of 40 to 80 years. Two million of these patients will develop symptoms due to chronic venous insufficiency.2
Patients frequently ask what caused them to develop varicose veins. They want to know if they will get more in the future, and if their children may be at risk for varicose veins. Many patients ask if they can prevent the development of future varicose veins after treatment or surgery. They are also increasingly aware that problems in the veins may be an indicator of risk for problems elsewhere in the vascular system, including problems in the arteries.
Risk factors for varicose veins can be classified as acquired/environmental or inherited. Acquired risk factors include age, obesity, pregnancy, sex and occupations that involve prolonged standing.3 Many patients will also have a family history of varicose veins. Several landmark studies show positive association between the occurrence of varicose veins and a family history.4-8 It is important to note that family history was self-reported by the patients, which may lead to bias.
 The Role of Genetics: A Look at the Studies
The Role of Genetics: A Look at the Studies
Epidemiological data strongly supports familial clustering for varicose vein disease. Up to 17% of patients with varicose veins are reported to have first degree relatives with disease.9 Research on the heritability of venous function measured by impedance plethysmography in twin pairs demonstrates that age and gender adjusted heritability for venous capacity is 30%, and for venous compliance it is 90%.10 This data supports a genetic basis for varicose veins.
A few global genetic studies that examine the genetics of varicose veins have been performed. A phenomewide association meta-analysis (PheWAS, a technique to study the diseases associated with specific genes) of connective tissue related disorders (pelvic floor dysfunction, abdominal hernia, varicose veins and hemorrhoids) found that varicose vein associations overlapped with hematopoietic conditions, namely activated partial thromboplastin time (APTT). The PheWAS study found that both varicose veins and hemorrhoids were significantly associated with a specific single nucleotide polymorphism (SNP, variation of a single DNA base pair), “rs735854”, in the gene encoding myosin heavy chain 9 (MYH9).11
Another study used gene chip arrays to study the global expression of 47,000 gene transcripts and 38,500 well-characterized genes in 10 patients with chronic venous insufficiency and 10 controls without chronic venous insufficiency. This study demonstrated that regulatory genes of arachidonic acid metabolism and mediators of the inflammatory reaction (HPGD) were over-expressed in patients with chronic venous insufficiency. Also, the regulatory genes for collagen production were down-regulated in veins affected by superficial reflux disease.12
In contrast with the population-based genetic approach taken in the two studies outlined above, family-based studies have been used to identify predisposing genes for varicose veins in the context of a syndrome. Varicose veins have been observed to be associated with a range of genetic syndromes. Chromosomal disorders such as Klippel-Trenaunay syndrome (KTS; translocation 8:14, 5:11), monosomy 14 and trisomy of chromosomes 7, 12 or 18 are associated with varicose veins.
Varicose veins are also associated with gene mutations in vascular Ehlers-Danlos syndrome (COL3A1, encoding type III collagen), Chuvash polycythemia (VHL, encoding von Hippel–Lindau tumor suppressor), Lymphoedema distichiasis (FOXC2, encoding the Forkhead Box C2 transcription factor), severe congenital neutropenia type 4 (G6PC3, encoding the Glucose-6- Phosphatase Catalytic Subunit 3), and one mutation in a family with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL; Notch3, encoding the Neurogenic locus notch homolog protein 3, mutation G1279T).
“Varicose veins are one of the most common medical conditions in the western world, with 23% (about one-fourth) of adults in the United States affected with disease.”
A Novel Study on Varicose Veins
Based on clinical experience, as well as prior population based and family-based genetic studies, we have initiated a novel study to identify specifically those genes that cause varicose veins. The number of individuals impacted by chronic venous insufficiency worldwide and the evidence suggesting a genetic etiology of varicose veins are compelling reasons for this research. The project is a close collaboration between clinicians with a dedicated venous practice, led by Dr. Sheila Coogan, and Dr. Dianna Milewicz, a leading geneticist with a proven track record of identifying genes that cause vascular disease.
Dr. Sheila Coogan is an Associate Professor of Surgery in the Department of Cardiothoracic and Vascular Surgery at the UTHealth McGovern Medical School at Houston. Prior to returning her native Houston, Dr. Coogan worked at Stanford for six years where she developed expertise in minimally invasive vascular surgery. The Cardiothoracic and Vascular department has expertise in unusual aortic pathologies—including aortic aneurysms, thoracoabdominal aortic aneurysms, and aortic dissections.
During her tenure at McGovern Medical School, Dr. Coogan also developed an interest in the biology of venous disease. She has a robust clinical vein practice that includes varicose vein treatment, venous ulcers, deep vein thrombosis, and chronic venous obstructive disease. Dr. Sheila Coogan and Dr. Dianna Milewicz have collaborated over the years, and while having coffee one day in the nearby Rice Village, Dr. Coogan told Dr. Milewicz that most patients with varicose veins had a family history of the disease.
This conversation initiated the collaboration to study the genetics of venous disease using the same template that Dr. Milewicz successfully demonstrated for aortic disease.
Dr. Milewicz has focused her career on identifying the genes that, when altered, predispose to vascular diseases. She has identified genes for thoracic aortic aneurysms, acute aortic dissections, and early onset strokes. She has received numerous honors and awards for her research, including the Antoine Marfan Award, the Doris Duke Distinguished Clinical Scientist Award and the University of Texas Presidential Scholars Award for Excellence in Research.
Currently, she holds the President George H.W. Bush Chair of Cardiovascular Medicine, and is Director of the Division of Medical Genetics and Vice-Chair of the Department of Internal Medicine at the UTHealth McGovern Medical School at Houston.
Dr. Milewicz is internationally-renowned for her success in identifying genes that cause familial thoracic aortic aneurysms and dissections (FTAAD). Her group has identified several genes for FTAAD using different genetic techniques. Positional cloning identified mutations in three genes causing FTAAD: TGFBR2, encoding transforming growth factor- receptor type II and ACTA2 and MYH11, encoding the smooth muscle specific isoforms of -actin and -myosin, respectively.13-16 A candidate gene approach was used to identify three additional FTAAD genes: TGFBR1 encoding transforming growth factor- receptor type I, FBN1 encoding fibrillin, and MYLK encoding myosin light chain kinase.17-20
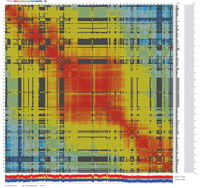
Dr. Milewicz’s group has recently turned to whole exome sequencing (WES) to identify rare variants in novel genes for TAAD and increase the pace of novel gene identification. WES provides an unbiased assessment of genetic variants in the protein coding regions of the genome. Since approximately 85% of causative mutations for Mendelian diseases are found in the coding regions or in canonical splice sites, WES is an efficient approach to identify causative mutations for these diseases.21, 22
 Important Advances in Technology
Important Advances in Technology
Commercial human exome capture arrays and next generation sequencing technologies are designed to capture and sequence approximately 97 - 99% of the exons and flanking introns that are in current genomic databases. Additionally, computer programs have been developed to map sequence reads to the reference human genome, identify genetic variants, annotate amino acid changes, predict the impact of an amino acid substitution on the structure and function of a human protein, and search minor allele frequencies in different populations using multiple publicly available databases, such as the National Heart Lung and Blood Institute GO Exome Sequencing Project (NHLBI GO ESP), 1000 Genome Project, and NCBI dbSNP databases.
Thus, WES has evolved into a robust technology for identifying coding variation at the genome-wide level and enabling researchers to identify causative rare variants predisposing to diseases rapidly and efficiently.
“Data from syndrome associated varicose veins provides evidence that many different genes can cause varicose veins. In other words, varicose veins are genetically heterogeneous.”
Parallel to advances in genetic technology, there have been advances in technology used to collect DNA samples for sequencing. State-of-the-art ”spit kits” (Oragene saliva collection kits, proprietary formulation) from DNA Genotek are now used for painless and facile collection of saliva samples to isolate DNA from patients. These DNA samples are stable at room temperature for several years.
Identifying Genes: Approaches and Plans
Data from syndrome associated varicose veins provides evidence that many different genes can cause varicose veins. In other words, varicose veins are genetically heterogeneous. This has been true of almost all common vascular diseases. To rapidly identify novel genes for FTAAD, another vascular condition with genetic heterogeneity, Dr. Milewicz has used two approaches and plans to use these same approaches to identify genes for varicose veins.
The first is the “trio approach.” This approach would identify patients with early onset of significant varicosities, but no family history of the condition, and then collect DNA from the affected individual and both unaffected parents. Whole exome sequencing would be performed for all three individuals, and then rare genetic variants identified (each individual has approximately 300 rare variants in their genome) to pinpoint new rare variants in the affected individual that are not present in the unaffected parents (de novo variants) or compound heterozygous and homozygous variants in a single gene in the affected individual (for recessive conditions).
The second approach is to use large families with evidence of autosomal dominant inheritance of varicose veins. Whole exome sequencing would be performed on several affected relatives and variants filtered for rare variants that are shared by all affected relatives. These twin strategies are used to identify rare variants in novel genes that predispose to varicose veins.
Conclusion
In summary, varicose veins have a proven genetic etiology. We initiated a study focused on identifying genes predisposing to a single defined phenotype of chronic venous insufficiency—large varicose veins. Two patient groups are the initial cohort in this study:
- Patients younger than 25 years of age with large varicose veins
- Very large families with at least three affected family members with large varicose veins
The ease of obtaining DNA from a genetic spit test will allow the study to be carried out on patients globally. We look forward to updating you with the results of our research as causative genes for varicose veins are identified, and we look forward to collaborating with venous specialists worldwide.
For more information regarding the study, contact Dr. Coogan here.
References:
- Hamdan A. Management of varicose veins and venous insufficiency. JAMA 2012 December 26;308(24):2612-21.
- McGuckin M, Waterman R, Brooks J, Cherry G, Porten L, Hurley S, Kerstein MD. Validation of venous leg ulcer guidelines in the United States and United Kingdom. Am J Surg 2002 February;183(2):132-7.
- Callam MJ. Epidemiology of varicose veins. Br J Surg 1994 February;81(2):167-73.
- Widmer LK. Peripheral Venous Disorders Basel III. Bern: Hans Huber; 1978.
- Hirai M, Naiki K, Nakayama R. Prevalence and risk factors of varicose veins in Japanese women. Angiology 1990 March;41(3):228-32.
- Mekky S, Schilling RS, Walford J. Varicose veins in women cotton workers. An epidemiological study in England and Egypt. Br Med J 1969 June 7;2(5657):591-5.
- ARNOLDI CC. The heredity of venous insufficiency. Dan Med Bull 1958 June;5(5):169-76.
- Matousek V, Prerovsky I. A contribution to the problem of the inheritance of primary varicose veins. Hum Hered 1974;24(3):225-35.
- Fiebig A, Krusche P, Wolf A, Krawczak M, Timm B, Nikolaus S, Frings N, Schreiber S. Heritability of chronic venous disease. Hum Genet 2010 June;127(6):669-74.
- Brinsuk M, Tank J, Luft FC, Busjahn A, Jordan J. Heritability of venous function in humans. Arterioscler Thromb Vasc Biol 2004 January;24(1):207-11.
- Salnikova LE, Khadzhieva MB, Kolobkov DS. Biological findings from the PheWAS catalog: focus on connective tissue-related disorders (pelvic floor dysfunction, abdominal hernia, varicose veins and hemorrhoids). Hum Genet 2016 July;135(7):779-95.
- Markovic JN, Shortell CK. Genomics of varicose veins and chronic venous insufficiency. Semin Vasc Surg 2013 March;26(1):2-13.
- Pannu H, Fadulu V, Chang J, Lafont A, Hasham SN, Sparks E, Giampietro PF, Zaleski C, Estrera AL, Safi HJ, Shete S, Willing MC, Raman CS, Milewicz DM. Mutations in transforming growth factor-beta receptor type II cause familial thoracic aortic aneurysms and dissections. Circulation 2005 July 26;112(4):513-20.
- Zhu L, Bonnet D, Boussion M, Vedie B, Sidi D, Jeunemaitre X. Investigation of the MYH11 gene in sporadic patients with an isolated persistently patent arterial duct. Cardiol Young 2007 December;17(6):666-72.
- Pannu H, Tran-Fadulu V, Papke CL, Scherer S, Liu Y, Presley C, Guo D, Estrera AL, Safi HJ, Brasier AR, Vick GW, Marian AJ, Raman CS, Buja LM, Milewicz DM. MYH11 mutations result in a distinct vascular pathology driven by insulinlike growth factor 1 and angiotensin II. Hum Mol Genet 2007 October 15;16(20):3453-62.
- Guo DC, Pannu H, Papke CL, Yu RK, Avidan N, Bourgeois S, Estrera AL, Safi HJ, Sparks E, Amor D, Ades L, McConnell V, Willoughby CE, Abuelo D, Willing M, Lewis RA, Kim DH, Scherer S, Tung PP, Ahn C., Buja LM, Raman CS, Shete S, Milewicz DM. Mutations in smooth muscle alpha-actin (ACTA2) lead to thoracic aortic aneurysms and dissections. Nat Genet 2007 December;39:1488-93.
- Loeys BL, Schwarze U, Holm T, Callewaert BL, Thomas GH, Pannu H, De Backer JF, Oswald GL, Symoens S, Manouvrier S, Roberts AE, Faravelli F, Greco MA, Pyeritz RE, Milewicz DM, Coucke PJ, Cameron DE, Braverman AC, Byers PH, De Paepe AM, Dietz HC. Aneurysm syndromes caused by mutations in the TGF-beta receptor. N Engl J Med 2006 August 24;355(8):788-98.
- Tran-Fadulu V, Pannu H, Kim DH, Vick GW, III, Lonsford CM, Lafont AL, Boccalandro C, Smart S, Peterson KL, Hain JZ, Willing MC, Coselli JS, LeMaire SA, Ahn C, Byers PH, Milewicz DM. Analysis of multigenerational families with thoracic aortic aneurysms and dissections due to TGFBR1 or TGFBR2 mutations. J Med Genet 2009 September;46(9):607-13.
- Wang L, Guo DC, Cao J, Gong L, Kamm KE, Regalado E, Li L, Shete S, He WQ, Zhu MS, Offermanns S, Gilchrist D, Elefteriades J, Stull JT, Milewicz DM. Mutations in Myosin light chain kinase cause familial aortic dissections. Am J Hum Genet 2010 November 12;87(5):701-7.
- Milewicz DM, Michael K, Fisher N, Coselli JS, Markello T, Biddinger A. Fibrillin-1 (FBN1) mutations in patients with thoracic aortic aneurysms. Circulation 1996 December 1;94(11):2708-11.
- Ng SB, Turner EH, Robertson PD, Flygare SD, Bigham AW, Lee C, Shaffer T, Wong M, Bhattacharjee A, Eichler EE, Bamshad M, Nickerson DA, Shendure J. Targeted capture and massively parallel sequencing of 12 human exomes. Nature 2009 September 10;461(7261):272-6.
- Turner EH, Lee C, Ng SB, Nickerson DA, Shendure J. Massively parallel exon capture and library-free resequencing across 16 genomes. Nat Methods 2009 May;6(5):315-6.


