 Chronic venous leg ulcers (VLU) are the result of endothelial damage and leukocyte activation, inflammation and changes in the microcirculation, which leads to persistent elevated venous ambulatory pressures, with eventual destruction of tissue integrity. Chronic venous disease and its severe form account for skin changes and ulceration, affecting 2-5% of the Western population (in the United States 2-3 million), with VLU affecting 1.5% of the Western population (in the United States 0.5-1 million).[1] Importantly, two million workdays per year are lost due to VLU, and may cause early retirement that affects up to 12.5% of workers with venous ulcers.[2] This puts the estimated cost of treating VLU at $3 billion annually.[3]
Chronic venous leg ulcers (VLU) are the result of endothelial damage and leukocyte activation, inflammation and changes in the microcirculation, which leads to persistent elevated venous ambulatory pressures, with eventual destruction of tissue integrity. Chronic venous disease and its severe form account for skin changes and ulceration, affecting 2-5% of the Western population (in the United States 2-3 million), with VLU affecting 1.5% of the Western population (in the United States 0.5-1 million).[1] Importantly, two million workdays per year are lost due to VLU, and may cause early retirement that affects up to 12.5% of workers with venous ulcers.[2] This puts the estimated cost of treating VLU at $3 billion annually.[3]
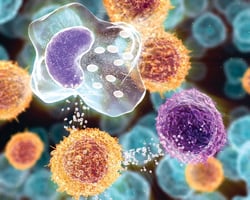
The pathophysiology of VLU is reflective of a complex interplay that involves genetic and environmental factors, injury to the endothelium and glycocalyx, leukocyte activation and inflammation, T-lymphocytes (particularly important in venous leg ulcer pathology), changes in the microcirculation, cytokine and matrix metalloproteinase (MMP) expression, sustained venous hypertension, and altered cellular function. For unknown
It is important that other standard aspects of VLU care are combined with compression to obtain optimal results, and in the discussion of the various adjuvant therapies applied to VLU directly, a summary of the significant results has been formulated to indicate if the treatment is beneficial in VLU healing (Table).reasons, the glycocalyx layer coating the endothelial layer is damaged. This leads to endothelial expression of specific adhesion molecules, including intercellular adhesion molecule-1 (ICAM-1), monocyte chemoattractant protein-1 (MCP-1), macrophage inflammatory protein-1a (MIP-1a), and vascular cell adhesion molecule-1 (VCAM-1, CD-106), with the expression and shedding of L-selectins and E-selectins.  The result: recruitment of leukocytes and leukocyte transmigration into the vein wall and valve, setting up an inflammatory cascade and production of several cytokines, including transforming growth factor-b1 (TGF-b1), tumor necrosis factor-a (TNF-a) and ilterleukin-1 (IL-1), as well as increased expression of MMPs. Chemoattractants and endothelial activation recruits leukocytes and causes diapedesis of these cells
The result: recruitment of leukocytes and leukocyte transmigration into the vein wall and valve, setting up an inflammatory cascade and production of several cytokines, including transforming growth factor-b1 (TGF-b1), tumor necrosis factor-a (TNF-a) and ilterleukin-1 (IL-1), as well as increased expression of MMPs. Chemoattractants and endothelial activation recruits leukocytes and causes diapedesis of these cells
into the dermal microvasculature, promoting an inflammatory response by macrophages and mast cells, with release and activation of cytokines and proteinases. Altered cell function enhances a state of vulnerability in the surrounding tissues, initiating specific changes associated with venous disease. Ultimately, persistent chronic venous insufficiency (CVI) perpetuates the inflammatory-proteinase state, leading to venous ulcer formation .[4,5]
The fundamentals of venous ulcer treatment is the correction of the underlying CVI with compression therapy. Understanding the science involved in the pathophysiology of venous ulcer formation, has led to the development of adjunctive topical treatments directed at the dysregulated inflammatory, cytokine and MMP expression, and molecular pathways that are dependent on growth factors. Randomized clinical trials are critical to determine the most effective evidence-based treatments for venous ulcer, and this review will address the important trials that have had a significant impact on venous ulcer healing.
Compression Therapy, Cytokines and VLU Wound Care
"> The successful treatment of patients with venous ulcers requires consistent compression of the limb to eliminate edema counteracting the venous hypertension underlying the inflammatory mechanisms outlined above. Essentially, all wound care dressing applied topically to the VLU are in conjunction with compression bandaging or garments. Based on multicenter prospective randomized trials, it is evident that high-strength compression (> 30 mm Hg) and multilayered compression methods are more effective than lower strength or single layered compression.[6]
The successful treatment of patients with venous ulcers requires consistent compression of the limb to eliminate edema counteracting the venous hypertension underlying the inflammatory mechanisms outlined above. Essentially, all wound care dressing applied topically to the VLU are in conjunction with compression bandaging or garments. Based on multicenter prospective randomized trials, it is evident that high-strength compression (> 30 mm Hg) and multilayered compression methods are more effective than lower strength or single layered compression.[6]
Many studies have demonstrated the benefit of compression stockings and venous ulcer healing.[7] Publication from the Cochrane database has unequivocally established that compression therapy heals VLU and prevents recurrences. After ulcer healing, compression must be maintained chronically to prevent recurrent ulceration. The impact of VLU recurrence when compression is not routinely used, has been assessed. In patients who were compliant with elastic compression stockings, 97% healed the VLU. In non-compliant patients, only 55% healed their ulcer. Notably, in compliant patients wearing compression, recurrences after healing occurred in only 16%, while in non-compliant patients the recurrence was 100% at 36 months.[8]
It is well-established that VLU have a significant number of cytokines present in the ulcer bed. The importance of compression therapy on modulating cytokine expression was studied in an elegant analysis of cytokine levels and VLU healing, where biopsies were taken before and at four weeks after compression, and studied by multiplex protein assay for a variety of cytokines. This clinical study determined that untreated ulcers typically display high levels of pro-inflammatory cytokines, including several interleukins, TNF-a, and Interferon-g (IFN-g).
After four weeks of multi-layer compression therapy, the levels of pro-inflammatory cytokines decreased significantly and the wounds began to heal. After compression, levels of TGF-b1 increased significantly as the ulcers improved. When specific cytokine levels were related to the percentage of healing of greater than 40% at four weeks, it was found that those with higher levels of pro-inflammatory cytokines, including IL-1 and IFN-g, healed significantly better than those with lower levels of these cytokines prior to compression. In addition, as the VLU healed, the level of the anti-inflammatory cytokine IL-1 Ra increased at four weeks following compression.[9]
The importance of this study was to demonstrate the inflammatory and anti-inflammatory cytokines present in VLU, and how compression therapy is able to modulate the expression and promote VLU healing. Future study will be required to assess if assaying cytokines from VLU can determine potential for healing and provide novel therapies such as cytokine stimulation or inhibition in non-healing venous ulcers.
The pathophysiology of VLU allows for the possibility of utilizing various adjuvant agents, biomolecules and membranes, growth factors, biologic skin substitutes, and non-biologic MMP inhibitors, to the wound bed in an effort to expedite healing.[10] It is important that other standard aspects of VLU care are combined with compression to obtain optimal results, and in the discussion of the various adjuvant therapies applied to VLU directly, a summary of the significant results has been formulated to indicate if the treatment is beneficial in VLU healing (Table).
The optimal VLU wound prior to application of topical biologic and non-biologic agents should have a good granulated matrix bed, and must be free of infection, necrotic tissue and wound exudates, as some of these variables may affect the success of ulcer healing.[11] Debridement to remove necrotic tissue should be performed frequently during clinic visits, and application of lidocaine gel is helpful for patient comfort during debridement. Large VLU wounds requiring extensive debridement should be performed in the operating room under monitored anesthesia care or under general anesthesia, to ensure complete removal on all non-viable tissue.[12] A primary wound dressing is selected based on the amount of exudate expected and the duration of the dressing before the next application. Most venous leg ulcers have heavy exudate, especially at initial treatment.
Therefore, foams, alginates, or other highly absorptive primary dressings are appropriate selections.[13] Cadexomer iodine and silver sulfadiazine have also been shown in randomized trials to reduce the venous ulcer area, and possibly important adjuvant treatment to compression. There is little data to suggest that one dressing is optimal for the treatment of venous ulcers.[14] An extensive review published in the Cochrane database in 2006 concluded that the type of dressing applied to the wound under compression had not been found to affect ulcer healing.[15] Similarly, while silver-containing dressings are applied to VLU, there is little evidence to suggest that they reduce the incidence of ulcer infection or accelerate wound healing. A randomized controlled study (VULCAN trial) compared the healing rate for venous ulcers treated with silver-donating dressings to standard dressing in 213 patients. No significant difference in wound closure between the two groups was noted.[16]
A recently published investigator-blinded randomized controlled trial evaluated the efficacy of a polymer, poly-N-acetyl glucosamine (pGlcNAc) nanofiber-derived technology (Talymed, Marine Polymer Technologies Inc, Danvers, MA), with properties of enhancing angiogenesis, granulation tissue, and epithelialization. The primary outcome of complete VLU healing at 20 weeks was greater for pGlcNAc applied every other week in conjunction with compression (86.4%; n=22), compared to compression alone (45.0%; n=20; P=0.005).[17]
Future trial will require larger sample size and follow up to determine the benefit of this new wound dressing in VLU treatment and recurrence rates. In numerous studies using various methods of compression, ulcer healing rates have consistently averaged 60-70% at 12-24 weeks of treatment. Specific evidence-based guidelines are lacking, and there is significant variation in practice patterns of wound and skin care management. Further randomized controlled trials are required to define skin and wound management in the adjuvant treatment of VLU.[13,18]
Topical Growth Factors in the Treatment of VLU
Several growth factors have been studied in patients with VLU to determine whether topical application would result in improved wound healing. A randomized controlled trial of 71 patients with VLU treated with PDGF-BB (becaplermin) gel compared to placebo gel found no difference in healing rates.[14] Another study evaluated 86 patients with VLU, randomized to treatment with autologous platelet lysate (which is known to contain PDGF) versus placebo and compression; however, no difference was achieved in time to ulcer healing for platelet lysate compared to the placebo.[19] In a double-blind randomized controlled trial, it was found that frozen autologous platelets placed on VLU have no effect on ulcer healing.[20]
In another double-blind randomized controlled study, recombinant human epidermal growth factor (rh-EGF) was applied to 17 patients with VLU and compared to a placebo in 18 patients with VLU for up to 10 weeks. Although rh-EGF was well-tolerated with no untoward side effects, there was no evidence of statistically significant improvement in venous ulcer size reduction or healing, nor re-epithelialization, when compared to placebo.[21] Another growth factor evaluated in patients with VLU was recombinant human granulocyte-macrophage colony-stimulating factor (rh-GM-CSF).
In this small double-blind randomized controlled trial of 60 patients, which were randomized to three groups (placebo, rhGM-CSF 200 mg or 400 mg ), they were injected in the peri-ulcer region weekly for four weeks or until ulcer healing, with all patients having four-layer compression bandaging. At 12-14 week follow ups, rhGM-CSF was found to significantly improve venous ulcer healing with no major side effects (placebo=19%; rhGM-CSF 200=57%; rhGM-CSF 400=61%; P=0.014).[22] In a promising study using recombinant human keratinocyte growth factor-2 (rhKGF-2, rhFGF-10, Repifermin) evaluated 94 patients with venous ulcers.
In this double-blind, placebo-controlled protocol significantly more patients achieved 75% wound closure at 12 weeks in the Repifermin group compared to the placebo group. In a subgroup analysis, patients with initial wound areas £15 cm2 and wound ages of £18 months also appeared to have a better effect.[23] Given that the studies on topical growth factor therapy treatment for VLU are small and with equivocal findings, and the fact that human recombinant growth factors are very expensive, there is no current growth factor therapy approved by the FDA to heal VLU.
Because the VLU environment is proteinase-rich, investigation evaluated if there is a growth factor deficit in venous ulcer tissue. In a study of tissue from 35 patients with VLU, levels of vascular endothelial growth factor (VEGF) were measured. Tissue samples were obtained from wounds in 18 patients undergoing other surgeries unrelated to venous disease for controls. They found that non-healing VLU display a consistently high level of expression of VEGF, both at the gene transcription and protein level. The study concluded that VEGF inhibitors or inadequate receptors may be prohibiting proper angiogenesis in venous ulcer tissue, but that it is unlikely that topical application of VEGF would improve healing.[24] Other studies have also determined that TGF-b1 and EGF are present in similar quantities in patients with VLU compared to control subjects.[25]
It is likely that topical growth factors do not achieve adequate levels for VLU healing for several reasons. Different growth factors and cytokines are required in a temporal fashion during wound healing, and applying a single growth factor is unlikely to provide stimulus for all the phases of wound healing. It may also be that the presence of pro-inflammatory cytokines inhibits the function of growth factors, and the presence of necrotic or infected tissue does not allow for proper growth factor function. And finally, the presence of serine proteases and proteinases, especially MMPs, likely degrade many of the growth factors that are necessary for proper VLU healing.[10]
Modulation of MMP in the VLU Microenvironment
MMPs have been demonstrated to be over-expressed in both the wound fluid and in tissue biopsies of VLU.[4] Therapies directed at modulating MMPs may have promise in ulcer healing. Oxidized regenerated cellulose/collagen matrix (ORC/collagen matrix) changes wound microenvironments by binding and inactivating gelatinases in wound exudates. A clinical study of patients with venous leg ulcers compared the levels of the MMP-2 in the wound exudate treated with ORC/collagen matrix (17 patients) or control hydrocolloid dressing (10 patients). The patients treated with ORC/collagen matrix showed a significant decrease in gelatinase activity compared with the control group as measured in the VLU wound exudate; however, there was no difference in the healing rates between the two groups.[26]
A dressing composed of a combination of collagen and regenerated cellulose (Promogran, Johnson & Johnson) has been developed based on its ability to bind MMPs in wound fluid in vitro. Several studies have found benefit in ulcers where Promogran decreases the ratio of MMP-9/TIMP-2 in tissue biopsy compared to ulcers treated without Promogran. Although surface area was reduced with Promogran, ulcer healing was unaffected.[27] The nano-oligosaccharide factor (NOSF) is a newer compound promoting wound closure through inhibition of MMP activity and stabilization of growth factors. A randomized study evaluated the NOSF versus Promogran matrix (oxidised regenerated cellulose, ORC) effect of VLU. Patients were randomized to either NOSF matrix or ORC treatment for 12 weeks. A total of 117 patients were included, with 57 patients treated with NOSF and 60 patients with ORC, and all receiving compression therapy. At completion of 12 weeks of treatment, NOSF had a better percent wound relative reduction over ORC (54.4% NOSF versus 12.9% ORC P=0.0286).[28]
In addition, VLU regression of greater than 40% was increased for patients with VLU of greater than six months duration compared to those with a VLU of less than six months. The study concluded that NOSF matrix is a promising option for the management of chronic VLU. A more recent trial of patients with VLU and treated with lipido-colloid technology (TLC) containing NOSF (TLC-NOSF), demonstrated that the relative wound area reduction was significantly higher for TLC-NOSF compared to only TLC (58.3% vs. 31.6%; P=0.002). In addition, TLC-NOSF increased the healing rate as well as the absolute wound area reduction (cm2).[29]
Human Skin Equivalents and Biologic Matrices in Treating VLU
Large VLU wounds that do not improve with a significant decrease in size over three to four weeks of treatment, or that have been present for greater than six months, may be considered for adjunctive healing methods. Apligraf, (Graftskin, human skin equivalent composed of a bi-layer of cultured fibroblasts and keratinocytes, Organogenesis Inc, Canton, MA), a living tissue equivalent, to accelerate wound closure. Apligraf is able to provide many of the growth factors and cytokines to help stimulate the wound bed provisional matrix. In a prospective randomized controlled trial of 240 patients with VLU, Apligraf with compression was compared to compression alone. At 24 weeks, 57% of the Apligraf group had closed compared to 40% of the compression alone group (P=0.02). However, the recurrence rates were similar. In a subset analysis, the study found a benefit of Apligraf in healing venous ulcers that were present for more than one year (47% vs. 19%, P=0.002), but there was no difference in ulcer recurrence rates.[30]
Recent work has focused on delivering growth-arrested neonatal fibroblasts and keratinocytes bound in a fibrin matrix, which can then be applied to the VLU wound bed as a spray prior to compression. A five-arm, double-blind randomized controlled trial with a 24-week follow up, demonstrated safety and efficacy of this novel delivery system, but longer term data is required to determine VLU healing benefit with allogenic cells applied topically.[31] Dermagraft (a human fibroblast-derived dermal replacement), demonstrated in a small non-randomized trial of 18 patients with VLU, found that 50% of the patients treated with Dermagraft with compression versus 12.5% of compression-only patients, had healed by the end of the 12-week study period—however, this was statistically insignificant.
The total ulcer area rate of healing and linear rate of healing was significantly improved in patients treated with Dermagraft (P=0.001 and P=0.006, respectively).[32] A recent VLU randomized controlled trial evaluating Dermagraft, consisted of 186 patients treated with Dermagraft with compression and 189 patients treated with compression alone. The primary outcome of complete healing at 12 weeks was 34% in the Dermagraft and 31% in the control group (P=0.23). Subset analysis found that patients with VLU of less than 12 months duration had complete healing at 12 weeks of 52% in the Dermagraft group versus 37% in the control group (P=0.029).[33]
The extracellular matrix (ECM) is a complex of many proteins, glycosaminoglycans, and growth factor receptors that allows for wound healing. An ECM derived from porcine small intestine submucosa (SIS Oasis, Healthpoint Ltd, Fort Worth, Texas) was developed. Using ECM SIS Oasis, a randomized controlled study of 120 patients randomized to SIS Oasis with compression (n=62) to compression alone (n=58), found to improve venous ulcers healing (55% vs. 34%, P=0.02). At a six-month follow up, there were no recurrences in the Oasis group.[34] A theoretical advantage of biologic skin and extracellular matrix is their ability to provide a scaffold for cell attachment and migration, and secrete growth factors such as FGF, KGF, GM-CSF, EGF, and TGF for cellular healing functions. However, one must also weigh in the number needed to treat to heal one VLU, the treatment efficacy, how many patients will continue to have an active VLU beyond 12 months (can exceed 50% of patients), and the cost associated with the treatment of biologic dressing.[35]
Conclusions
Chronic venous ulcers have an underlying etiology of endothelial dysfunction, inflammation and increased ambulatory venous hypertension, with microcirculatory abnormalities and proteinase activity. Basic scientific knowledge has elucidated our understanding of important molecules and pathways that include cytokines, growth factors, and MMPs. These scientific studies provide an opportunity to intervene at multiple levels, with the ultimate goal of finding a cure for advanced venous disease. Compression therapy is a proven method for healing VLU, and is paramount to reduce recurrences. Various wound dressing therapies should always be applied along with compression therapy when considering VLU healing. There is no single dressing (non-adherent, hydrocolloid) that is superior, although there may be improved healing with poly-N-acetyl glucosamine polymer. But larger trials are needed to establish unequivocal efficacy in VLU healing. Autologous platelet preparations and silver dressings add expense and do not increase VLU healing. Unfortunately, clinical studies with growth factors have not yielded overwhelming positive results for VLU healing. Inhibition of MMPs may have some benefit in helping to heal VLU, but further studies are required to determine which MMPs in the VLU need to be altered to provide the proper healing environment. Biologic human equivalent tissue and porcine matrix demonstrate efficacy in treating venous ulcers, and should be considered for difficult-to-heal VLU, but one has to weigh the efficacy and cost when providing such treatment. Future clinical trials should focus on modulating multiple pathways of venous ulcer pathophysiology, including restoring function to the endothelium and glycocalyx, modulating the inflammatory response, as well as cytokines and growth factors, and inhibiting degradative MMPs.
References


