I had the very good fortune to interview Dr. Kistner on Memorial Day, which seemed profoundly more significant after speaking with him and hearing his story. It wasn’t long into our discussion that it became clear as to why Dr. Kistner is highly regarded as a leader in the field by all of his peers. With a relaxing style that is no doubt aided by his relocation to Hawaii almost 50 years ago, he is quick to laugh and patient in his speech. He embodies the work ethic that built a nation, and has been instrumental in the growth of the specialty. Dr. Kistner’s acute perspective on veins and intriguing historical recollections on the growth of phlebology is sure to entertain, educate and provoke thought. Read on for a clinic in leadership and ethic from a man who personifies these terms.
Dr. Kistner, you have a storied career in medicine and in the treatment of venous disease. What is it that made you choose to go into medicine?
From my earliest memories, I knew I was going to go into medicine. It’s all I can recall ever wanting to do. My father was a doctor—an ENT specialist in St. Louis, Missouri. He had four boys and three of us became doctors. It must be in the blood somewhere (laughs). My oldest brother, who was 13 years older than I, was a doctor in the military and gave his life at the Battle of the Bulge in WWII. My second brother, who was four years younger than our oldest brother, went through medical school during WWII and served in the U.S. Army for a couple years after. He practiced medicine in St. Louis until he was 85 and passed at 92. Our third brother was a businessman in St. Louis. He was the only one of the group who didn’t share the passion for medicine and chose the more normal way of life (laughs). He passed of a ruptured aneurysm in his early eighties. And then there was me.
We were all Jesuit trained at the University of St. Louis. I left St. Louis after my training there at age 30. I went West and never returned to live in the Mid-West. I was drafted for two years in the Air Force and stayed in California for an additional two years in practice of general surgery in Santa Barbara, California, then did a vascular fellowship at the Cleveland Clinic for 18 months and fell in love with the “big clinic” practice of medicine.
When I finished in Cleveland, I had the opportunity to come to Hawaii from Dr. Niall Scully who was one of my senior residents and a major role model in my life. He was practicing with the Straub Clinic in Honolulu, where I subsequently became the first trained vascular surgeon in Hawaii. It was an opportunity to come out and explore new fields in a fantastic place to live.
How did you come to choose vascular surgery/venous disease treatment as your focus after starting out in general surgery?
In my general surgery training there were elements of vascular surgery, but in those years, the early 1950s, a lot of the surgeries were not successful. I joined the U.S. Air Force as a general surgeon and went to Santa Barbara and practiced for a couple of years. During that time I decided that I wanted to do something more specialized in a developing field. There were several emerging fields at the time; pediatric surgery, thoracic surgery and vascular surgery, to name a few. I found an opportunity to train in vascular surgery at the Cleveland Clinic and it was a wonderful field to get into. It was just coming out of the woodwork at the time. In fact, it moved so fast that after I left training—which I thought was great and had great results—I found that many of the things I learned in training were already changing. This was a field of rapid change, and I was fortunate to be a part of it from its early development.
"You don’t invent anything; really, you simply build off of something that is already there."
I’m curious, what made you decide to join the Straub Clinic and move to Hawaii? Was this a difficult decision for you or the opportunity of a lifetime?
Yes, for me it was the opportunity of a lifetime. After doing general surgery for four or five years, I wanted to sub-specialize, and I found this wonderful atmosphere in the world of clinical medicine at the Cleveland Clinic. There was a national expert in every field whom you could call to consult on patients in a magnificent way. I was sold on clinic medicine as opposed to academic or solo practice.I had also been on the West Coast and liked the West. I had visited Hawaii, and when a friend invited me to Hawaii to do vascular surgery I thought, “Wow, clinical medicine and a wonderful place to live!” So I chose to make the move to Hawaii and never looked back.
When I came to Hawaii, a lot of people told me not to go because Asians do not have a predisposition to arterial disease, so after I arrived I started by doing some general surgery. The clinic quickly informed me that I was there to do vascular surgery and would not need to help with the general surgery (laughs). So I began to focus on venous disease and found a neglected field.
What is like to practice in Hawaii? Are there certain challenges or cultural elements that make it different from practicing on the mainland?
Every day is a beautiful day (laughs). There are a variety of people which makes practice challenging and interesting. Hawaii did not have a medical school until just before I arrived, and that was a two-year school that eventually became a four-year school. As a result, people who practice medicine here have been educated all over the United States so there was a mixture of great, well-educated people. That was stimulating.
The practice of medicine—the practice of everything—may be a little slower here, but everything is electronic now so you can educate yourself here as well as you can anywhere else. I had everything I wanted; great living conditions, a busy practice and the time and stimulation to follow my academic pursuits at the clinic.
"The thing about veins is that it’s kind of the “armpit” of vascular disease, and by that I mean people don’t pay enough attention to it. It’s an orphan and it has not been developed."
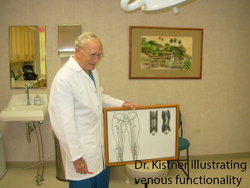
Tell us about your early experiences with valve repair.
While I was casting around looking for things to do in vascular surgery after I arrived in Hawaii, I came across a patient who had a clinical problem in his veins. I had been doing a lot of reading about Veins—at that time I was influenced by a paper on deep venous valve interruption by a surgeon named Robert Linton who was a famous vascular surgeon in Boston. My middle name is Linton, so I guess I related to his writings (laughing). Anyway, I was trying to emulate some of the stuff he was doing and came across this opportunity to fix a valve in this patient’s veins and it was successful. That was a career changer for me. From that point on, my life became something of an effort to explore and share the field of deep venous surgery. Looking back, it seems like a bunch of accidents that occurred, ultimately leading me to where I wanted to go.
It’s a funny thing about accidents. They seem like it at the time but upon reflection it appears that everything happens for a reason.
You don’t invent anything; really, you simply build off of something that is already there. And that’s what happened to me. When I fell into fixing that valve, there was so much serendipity in that it was unbelievable. It was not a matter of intense study in doing discovery—not at all (laughs). It was an accident that happened and was successful the first time. The subsequent development of deep venous surgical treatment in the controversial world was what really dominated my life—my academic life and much of the rest of my life. I have traveled all over the world and have done all kinds of things, and it is still going on. This is still very much an emerging field and still in its development.
The vascular world seems analogous to the software world, where technology and thought is constantly evolving. But I guess that’s common for any emerging industry or technology regardless of type.
The thing about veins is that it’s kind of the “armpit” of vascular disease, and by that I mean people don’t pay enough attention to it. It’s an orphan and it has not been developed. To this day, there is still enormous ignorance about it throughout the medical profession. It’s a serious matter that most medical schools don’t teach about venous disease at all, so physicians who come out of school don’t have any background in it. Their knowledge is gained by what they accrue in the post educational arena, and that is what gives them whatever appreciation of it I they may ultimately achieve. The arteries are a fascinating and wonderful field of development, but when it comes to the veins they are harder to understand. They are slower in development and much less exciting, and yet they are a constant source of trouble for about a quarter of the population. And that’s a big deal. It’s why this has been a lifelong crusade for me.
And making progress thanks in large part to you and the passionate doctors in the field of veins who are championing education at all levels. Please tell us about your early work with RF ablation and share your thoughts on how it progressed.
My introduction to RF ablation was in 1995. I was coming back from an American Venous Forum meeting and someone invited me to stop by Stanford and talk to an investor who had invested in the first endograft for aortic aneurysm. This fellow wanted to create a simple, minimally invasive way to make deep vein valves functional again... He detailed a young, partially-trained surgeon whose business was to develop ideas who worked on it for a couple of years. When he came back, he was kind of embarrassed. He said he had a way to maybe shrink the vein around the valve using radiofrequency current that might get the valve to work again. So, that led to an experience of working clinically with patients. We actually did shrink some veins and got some partial results.
One day we were at another meeting at the AVF where they had an animal lab and were showing us how to use this radiofrequency to shrink the valve in the experimental animal. During the demonstration the presenter made a remark that “you know, if you just shrink it a little harder the vein will shut down.” And suddenly, I think half of us in the room got the idea at the same time, we realized this was a minimally invasive way to treat varicose veins! That was around 1997. After a couple more years of development they came out with the first iteration of the VNUS Closure system in late 1999. Initial studies on it were encouraging; with time and experience a second iteration of the catheter was introduced, which is the one we use now. So RF ablation really grew out of an endovascular approach to make a deep venous valve work by scarring it. I don’t think many people know that history!
The man that grew the company, Brian Farley, brought it along beautifully. Coincidentally, at about the same time, the laser approach appeared and ran a collateral path of development. I really don’t know the inner story of EVLT. So now we have two methods of effectively treating the superficial veins with minimally invasive thermal techniques.
"People think of veins as the tail end of the circulation system. In a way, that is true since it is the return of half of the circulation but there is an enormous lack of knowledge to be plumbed for the researcher or clinical specialist."
What an amazing piece of history in the advancement of non-invasive varicose vein treatment.
This was really a turning point in venous disease because both thermal techniques were a practical way of producing a quality end result. Vein stripping was too traumatic for many patients to accept. It was the right thing to do physiologically but the wrong way because it was more traumatic—and perhaps because it had the unfortunate name of stripping. People want the simple approach and appreciate the “walk in and walk out” methods of treatment for their varicose veins.
To say you are well published, or have contributed to the field of phlebology via presentations, would be a vast understatement. Are there any presentations or published papers that you are most proud of? Any that you feel should be required reading for physicians who treat venous disease?
I think the best way to know how my thinking evolved was more from the chapters than the original presentations. When you write a chapter there is room for thought development and background, with reference to the research for developing new things.
In 1994 at a combined meeting, we noticed that people were talking about venous disease but they didn’t have the full range of essential elements to reference. To address this deficit, Bo Eklof, with whom I worked closely for 12 years, and I organized a group of experts from around the world under the auspices of an ad hoc committee of the AVF at a meeting in Hawaii later in 1994. Bo is a tremendous personality and was able to draw people from all over the world to this meeting. This meeting produced the CEAP (Clinical, Etiologic, Anatomic & Physiologic) Classification for venous disease. This is now the dominate standard classification around the world for chronic venous disease. Every world expert we invited to participate said “I’d like to work on that, there is a real need.” So there was a real hunger for this sort of thing. I guess timing is really important in whatever you do, and it just happened that everybody came together and fired from their knowledge base, and the leadership brought it out into an organizational thing.
I believe the CEAP classification will direct thinking and allow correlation of its disparate elements into a lifelong story about the development of chronic venous disease. The background of CEAP came largely out of frustration in early working with the complexities involved in study of the deep system. It is, I think, one of the most important developments that I have ever had a part in.
That is an incredibly significant contribution.
The CEAP system exists at a pretty basic level, not a very sexy level. People talk about the six clinical stages enumerated in CEAP, but that is just the cream on the top. What’s underneath that is the cause of chronic venous diseases (CVD) and the way it develops into advanced stages leading to ulceration and disability over time. I really think over the next decade or two the full story of CVD will continue to emerge and will be partially stimulated from this classification. This will require putting real data together that will come out of basic, as well as clinical science. And the basic science is going to play a major role in how we understand all this, with the role of inflammation and how it cascades, along with venous insufficiency.
Several years ago you were featured as one of the 25 most influential phlebologists in VEIN magazine. In that interview you cited a lack of knowledge of the natural history of acute and chronic venous problems as both contributing to the progression of venous disease and a major challenge in your work. Has this improved? If not, how do you feel it can be improved?
That’s really changed. A lot of that has been filled in by demographic studies that have been repeated. One study was in Bonn Germany by Eberhard Rabe, and another was the Edinburgh Vein Study. They had six- and 13-year follow-ups respectively of a mass of patients. Now we have quite a clear picture of chronic venous disease that is proven to be a progressive, degenerative problem.
These studies satisfied some of the criteria of CEAP, so when we start to put everything together this whole picture emerges of very slow, progressive phenomenon of venous hypertension resulting not only in vein disease but in skin changes and leading to ulceration.
At the AVF think-tank meetings in Hawaii, we came up with the concept of 50% reduction of venous ulcers in a decade in the United States. Well, that’s not possible but the thinking is possible to regard venous ulcers as something that is largely preventive with proper care. So this is all coming together as a big story involving education, understanding, proper diagnosis of venous disease as it develops, justification of treatment at various levels and minimization of treatment. One can see all of this coming together now and having some headway. They say with arterial disease you may lose a limb, but with venous disease you may lose use of the limb. It’s the challenge between talking about life and death as contrasted to the quality of life.
Tell us about your involvement in and experience as past president of the AVF and AVF Foundation.
I was invited to be one of the founding members of AVF and that was exciting. I was the eighth president, and at that time the AVF was in dire economic trouble for survival. The first thing I heard was that the company that was helping organize the AVF said we could not afford them and that they were bowing out. This led to an intense involvement in taking a look at what we were doing. We were running a venous forum and that’s what we were designed to do. We wanted to get people together to talk about veins and talk about publications. When we started out we thought, ‘can we ever get enough people and research together to have an annual meeting?’ We were saved by industry that came forward with funds—mainly the stocking industry. They believed in it. And we got an advisory group that helped with development. But development was slow, progressive, and we focused on increasing the size of the organization in terms of membership, both professors and practitioners.
Recently, the organization realized that it needed to reorganize itself if it wanted to do things that impacted the practice of venous disease treatment, like screening patients, registries, and overall more effective management. This has been ongoing for the past few years, and there is a progression of leadership that I think will function more effectively with commitment to certain principles and carrying them out. During my term, it was a matter of finding ways to survive and examining what we were doing so we could make appropriate changes. Today, the AVF is accepting responsibility to try and lead change that will affect society in a more general way.
Are there any other organizations you are highly active in?
I have always been involved with the local, regional and national societies and am still active at a minor level in the AVF and as an honorary member of the American College of Phlebology. Early on I was active in the American College of Surgeons and the Society of Vascular Surgery and International Cardiovascular Society where the early publications of deep vein surgery were first presented and nurtured, you might say. Now it’s focused down to venous disease.
What wisdom can you impart upon young physicians who have or are interested in pursuing the treatment of venous disease?
People think of veins as the tail end of the circulation system. In a way, that is true since it is the return of half of the circulation but there is an enormous lack of knowledge to be plumbed for the researcher or clinical specialist. And it ranges from the most basic science through all levels of care. For a career, it should be a choice for many people. It doesn’t involve life and death the way arterial vascular disease does but neither do arthritis and many other diseases. I think the long-term development really belongs to the general medical field as one of the more frequent and life-impacting chronic debilitating diseases in which the surgeon and the venous specialist will play an integral role of intervention as needed. Now that we see what the disease is, there are a lot of stages along the way where quality of medicine, if done correctly, will prevent more severe stages like ulcers.
I understand that you serve as a mentor for many younger vein specialists. Can you provide us with some examples of how you are serving as a mentor and the significance that mentoring has brought to you both professionally and personally?
I am so fortunate to have had such outstanding associates who have worked with me. Gene Ferris, Bo Eklof, Fedor Lurie and Elan Masuda are all colleagues whom I learned from and leaned on. I found out a long time ago that the best way to be successful is to associate with surgeons who are much smarter, turn them loose and support their progress. I’ve mentored many young people who have become physicians and some have gone into the vascular field. At Straub, we had a research and education foundation that developed training with residents and college students to bring them into the medical field and give them the experience of what it’s like to be a doctor. I think the most refreshing thing is to be trying to teach and talk with these young minds that are so great and lead you in different ways that are not predictable. Its’ the most stimulating thing you can do.
Do you have any closing thoughts for the physicians and venous disease specialists who read VEIN?
For me to spend so much time committed to this field, it takes support at home. There is a large sacrifice from family. Today, things are about quality of life. I think the world has changed. In our day, quality of life was being good in your field. My wife is very permissive with what I do with my hours, and that has allowed me do what I love. Without that, a lot of this doesn’t happen for me.


