Venous reflux refers to the abnormal backing up of blood in the veins. When blood flows backward in the veins, a person is then known to have venous insufficiency (also called chronic venous insufficiency or CVI for those for whom reflux is an ongoing concern). Venous insufficiency is a common medical condition that underlies most of the clinical presentations of venous diseases, such as varicose veins, swollen and achy legs, and venous ulcers.
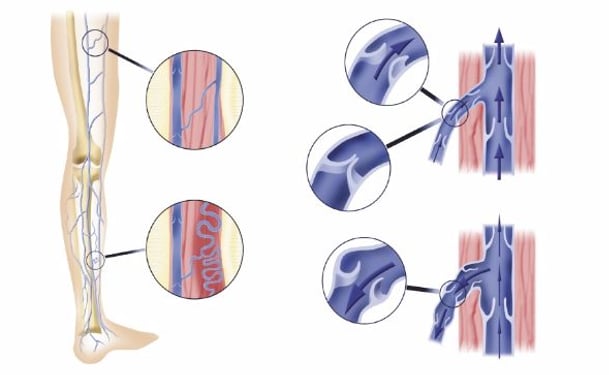
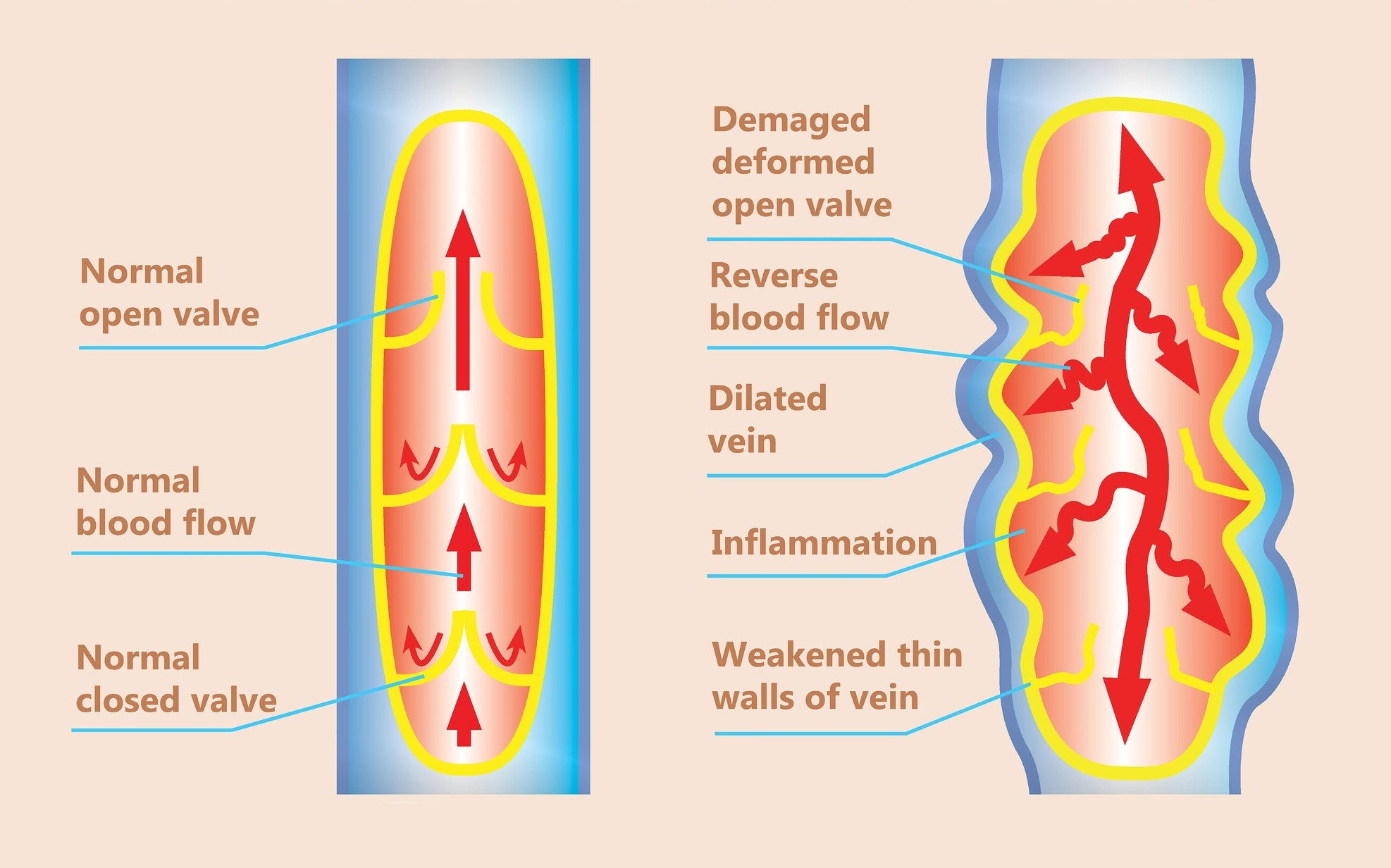
In healthy human circulation, the heart pumps blood carrying oxygen down through the body through the arteries; oxygen-depleted blood moves back up to the heart through the veins. Aided by the contraction of the calf muscle, blood in the veins moves against gravity.
Vein valves, which are small flaps attached to the inside of the vein walls, allow blood to flow upwards, and are key to vein health.
In healthy veins, valves are one way, meaning they allow the blood to move upward and then close so blood continues to move in the right direction. When veins are unhealthy, the valves become weak, and instead of closing, their laxity allows for two way blood flow. This causes venous insufficiency or CVI. See the illustration below.
Symptoms of venous insufficiency
CVI causes several symptoms ranging from mild to severe.
Pain often accompanies the symptoms of venous reflux. Sometimes legs can feel itchy, sore, or heavy. In severe cases, you may develop a venous ulcer (a wound by your ankles)
Diagnosing Chronic Venous Insufficiency
Your doctor will take a complete medical history and physical exam, taking special note of any changes in your skin temperature, color, and texture. Your doctor will also check the pulses in various places throughout your circulatory system.
After a physical exam, if your doctor suspects you have venous disease, you will then have a venous reflux exam. In this simple test, also called a duplex venous ultrasound, a sonographer or your doctor uses a handheld transducer to evaluate vein function, check for venous reflux and ensure there are no blood clots, blockages or other conditions.
The Role of CEAP Classification
The Clinical, Etiology, Anatomic, Pathophysiology known as CEAP classification is a system doctors use in the diagnosis of venous insufficiency. Venous disease is classified by the severity of symptoms. There are six levels of severity.
- C0 - No visible signs of venous disease
- C1 - Spider veins (known medically as telangiectases), which are less than 1 mm in diameter or reticular veins (also known as feeder veins), which are larger than spider veins, but not as large as varicose veins.
- C2 - Varicose veins (dilated veins larger than 3 mm in diameter)
- C3 - Swelling (known medically as edema) without skin changes
- C4 - Skin changes: A = Pigmentation or eczema; B = Lipodermatosclerosis (hardening of the skin) or atrophie blanche (a type of scar)
- C5 - Healed leg or ankle ulcer
- C6 - Active leg or ankle ulcer
Treatments for venous insufficiency
Treatment of venous insufficiency begins with an accurate diagnosis and finding the source of the venous reflux. Once reflux is detected, treatment will focus on removing the vein with the faulty valves, so that blood flow reroutes to healthy veins.
Venous insufficiency and lifestyle changes
Part of your treatment plan for venous reflux may include making healthy lifestyle choices that promote healthy venous circulation. Maintaining a healthy weight, eating healthy nutritious foods, and exercising regularly will help keep your blood circulating.
Walking is an especially good form of exercise. If you are sedentary most of the day, taking breaks to walk or move your body can encourage circulation.
If you stand for long periods during the day, take breaks to sit down. Putting your feet up will reduce swelling and inflammation.
Compression garments are often used either as the primary therapy for venous reflux or in conjunction with other therapies. Compression socks (above and below the knee) or compression pantyhose can help maintain venous blood flow. More potent forms of compression therapy are also available in cases of severe venous reflux.
Procedures for treating venous reflux
To treat venous disease, doctors remove the damaged vein(s) from your body. Vein removal can occur through several treatment modalities aimed at closing off and shrinking the damaged vein so that blood reroutes to healthy veins.
Which treatment method your doctor uses depends on several factors such as the diameter of the vein, its length, its location in your body, the tortuosity (meaning whether it twists and bends repeatedly), and the severity of your condition.
Venous insufficiency procedures fall under one of three categories:
- Thermal Tumescent (TT) modalities include radiofrequency or laser ablation. These treatments use heat and a tumescent (a chemical compound that produces anesthesia).
- Nonthermal Nontumescent (NTNT) modalities include ultrasound-guided foam sclerotherapy, mechanochemical ablation (also known as MOCA and commercially known as Clarivein). Most recently cyanoacrylate glue (known commercially as VenaSeal) hit the market. These modalities do not rely on heat and do not require a tumescent.
- Nonthermal Tumescent (NTT) includes vein stripping with tumescent.
Venous reflux risk factors
You may be at higher risk for venous reflux to occur if you:
- Have a family history of venous disease
- Stand daily for long periods of time — especially in physically demanding careers such as nursing or teaching
- Have been pregnant, or have experienced multiple pregnancies
- Are a woman
- Are obese
- Have injured your leg or ankle
- If you are elderly
To learn more about chronic venous insufficiency and the role of venous reflux, watch this illustrative video.