The landmark ATTRACT trial studied the use of endovascular therapy to prevent post-thrombotic syndrome. Now, a secondary trial known as C-TRACT wants to see whether this same therapy can reduce disability and improve quality of life in patients who've already developed thrombotic disease.
Dr. Suresh Vedantham, a principal investigator on both trials, joins Dr. Steve Elias to discuss the scale of the trial—from the patient types they're looking for and the partnerships that have been forged to find them, to testing options and the endpoints they'll measure.
 Steve Elias: C-TRACT starts with the letter c, and you had a trial that started with the letter a. Is this trial a continuation, or is it looking at a completely different pathology?
Steve Elias: C-TRACT starts with the letter c, and you had a trial that started with the letter a. Is this trial a continuation, or is it looking at a completely different pathology?
 Suresh Vedantham: It's looking at a different phase of the same condition. Whereas ATTRACT, the first trial, was focused on the use of endovascular therapy to prevent post-thrombotic syndrome, this study is focused on once patients have the disease how can we reduce their disability, improve their quality of life, improve their symptoms, and can endovascular therapy play a role there. So, that's what this study is focused on.
Suresh Vedantham: It's looking at a different phase of the same condition. Whereas ATTRACT, the first trial, was focused on the use of endovascular therapy to prevent post-thrombotic syndrome, this study is focused on once patients have the disease how can we reduce their disability, improve their quality of life, improve their symptoms, and can endovascular therapy play a role there. So, that's what this study is focused on.
Steve: There are many people out there already who say, "yeah, of course, I can help these people. I can just angioplasty them, stent them, do whatever, and these patients with chronic disease they do fine." Why do we need a trial?
Suresh: There are a number of reasons. First, in terms of the immediate results you get after some of these procedures, they indeed can be satisfying for providers, for patients. But in terms of the long-term, we do know that over time there are patients who develop narrowing or occlusion of their stents. There could be other issues that may pop up in the long run. There could be either continued improvement of the treatment effect versus some erosion of the treatment effect, and these things haven't really been characterized or quantified relative to the risk of the procedure. It would be great to know what's the level of benefit that's sustained relative to the risks.
The other reason to do it is that there is a lot of attention nowadays on expensive treatments from the people who paid for them. Developing a strong evidence base is very important to be able to ensure that we can deliver quality care to our patients and that they have access to it.
Patient characteristics
Steve: Who are the type of patients you're looking to answer the questions of the C-TRACT trial?
Suresh: The patients we're looking for are those who have had a previous DVT, a previous blood clot, have developed post-thrombotic syndrome, and the disease is of at least moderate severity. So, it actually affects their daily living in a significant way. And they need to have obstruction of the iliac vein, which we characterize as either total occlusion or at least 50% narrowing.
Steve: Let's get down to the clinical things. Someone comes to your office and says, "Doc, I had a DVT five years ago. I'm having trouble working, my leg is swollen. When I walk, after a little bit I get this bursting pain, et cetera." Or, patients who have had ulcers, secondary to chronic disease, as well. Those are the kinds of people you're looking for? Do you think there's more of those people around who are having significant symptoms, versus people who you were looking for in the ATTRACT trial?
Suresh: We know that there's a lot of them around, let's say it that way. ATTRACT was a thrombolytic treatment study, and therefore you needed to find people pretty soon after when they were diagnosed with a blood clot. Whereas, with this condition, many people have had it for many years. There is a large population of patients out there living with this disease. It's affecting their quality of life, and we wanna be able to find the best ways to improve that quality of life. We do think there is a significant share of people out there.
Study recruitment
Steve: How do you propose to find these people? What various ways are you going to employ in the trial to find these people?
Suresh: We’re using different mechanisms. First, there are the obvious routes of referral, where people with the condition present to different kinds of providers. We have 22 sites around the country that have kind of multi-disciplinary venous treatment programs. Generally speaking, they have an endovascular physician who does procedures. They have a medical physician that oversees anti-coagulant therapy—someone there who knows about compression therapy, as well as a wound or ulcer clinic. Now, we are encouraging all of them to make their local hematologists, vascular surgeons, vascular internists, phlebologists, interventional radiologists aware of the study. I think that we've largely achieved that at these centers.
But we're going quite a bit further than that. We have forged partnerships with a number of organizations around the health care arena, around venous disease, and they're helping us advertise the trial to a much larger swath of providers. We will also be using our electronic health records in these health systems—once again with IRB approval—to screen medical records to identify people who might have the condition that might want to have it treated. This is gonna be a long-term initiative. Again, this is a large NIH trial, and we will be successively increasing the intensity and diversity of our approach to finding patients.
Steve: Walk me through a little bit of what you've been presenting. You were nice enough to give me some of your slides to present at the AVLS meeting in November 2018. Talk to us about the electronic type of recruitment that you have.
Suresh: Most of the centers in the study have an electronic health record system nowadays, whether it's EPIC or Cerna, or whatever. And we have developed search terms that they can utilize to screen within their health care systems, and in their medical records, to identify a large number of patients.
In addition to that, we have developed a smartphone app. It's available both in the Google Play, as well as the Apple stores now, and you can download it. Our hope is that providers who see these patients will download the app and then they will have the ability to, in a completely privacy-protecting way, notify our coordinating center that they have a patient who might qualify. What we will do then is call the provider's contact number that they provided on the app and find out, "okay does this sound remotely reasonable?" We'll connect them up with the nearest study site, and then they can go in and help engineer that connection. The idea being that we're not dependent on just the patients who present to 22 hospitals, but we really are accessing a much larger range of patients.
Steve: What I liked about this was yes, you're gonna get to a larger range of patients hopefully, but it is a relatively painless procedure for the physician. Once they identify the patient, it's not like they gotta fill out all kinds of stuff and that type of thing. They need you to supply some basic information and then the call center, which will do most of the work. That to me is a very unique thing. This is not something that's been around that often with any other trial, at least not that I'm aware of.
Suresh: That's right. There probably are a few trials out there that may use something like this, but certainly in NIH trials, we haven't heard a lot of it being done. NIH is very excited and interested to see how this plays out.
When you get on the app, you answer three quick questions and provide one contact telephone number for a person we can reach—that's it. The idea is that a provider can do it without breaking stride.
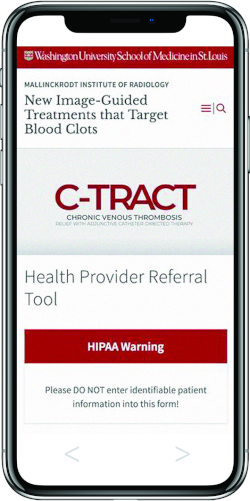 We're not saying go back to your computer and find our contact info or our brochure for our protocol. The idea is that it's in your pocket, you don't have to stop what you're doing. You can do it very quickly, and really the amount of work that you have to put into it in the middle of your busy day is minimized.
We're not saying go back to your computer and find our contact info or our brochure for our protocol. The idea is that it's in your pocket, you don't have to stop what you're doing. You can do it very quickly, and really the amount of work that you have to put into it in the middle of your busy day is minimized.
Steve: Have you considered some chronic disease patients know they have a blood clot most of the time, and sometimes they don't, but they know they may have had a blood clot in the past? They know their legs bother them, they know if they've had an ulcer. Have you considered rolling this out to the public, so to speak, in a way that they can access?
Suresh: We are planning on doing it. We're thinking about making sure there's information available on some of the forums (online forums) that are out there that tend to attract DVT, post-thrombotic syndrome, and venous patients in general. We have a social media coordinator here at Washington University. We have met with that person to get some guidance on most effective practices and most compliant practices to make sure we can do it in a way that everybody's happy with. But we absolutely will be doing that. I think it's a great idea.
Something that's even maybe more impactful than just us reaching out is the fact that, again, we've got six partner organizations. Remember, we're researchers and we learn to communicate. Some of these organizations, really, a big part of their role is communicating. We’re going to leverage their expertise. The fact that they've already built up populations of laypersons who are interested in venous disease, who may have relatives affected by it, means we can try and get the information out. And really, they're gonna be the ones who put a lot of the information out there. They're very excited about it, which we really appreciate.
Steve: Vein disease is a self-diagnosed disease most of the time by the patient, and it's very prevalent. So are you anticipating that recruitment may not be as difficult as the ATTRACT trial, or do you think it's gonna be around the same?
Suresh: I think it's gonna be very difficult. I mean, I think that these things are always difficult. When you're doing trials that are comparing a more invasive treatment with a less invasive treatment, I think right there that creates quite a bit of challenge in getting these things done. The patients need to feel like they're okay with the study, deciding which treatment they get. That means the providers and people they talk to have to be conveying that message. Both consciously, as well as subconsciously, as providers we do sometimes convey our biases or our general inclinations to a patient. We tend to be pretty opinionated people. And so on any given patient, even if we believe in both treatments, we might have a feeling of which one we think might be better for one patient. That's always challenging to present things in a really balanced way.
Testing treatment options
Steve: You bring up the treatment options. What are the choices, so to speak, that patients can be randomized to?
Suresh: Patients will be randomized to receive or not receive endovascular therapy. What all patients in both study arms are going to receive is standard compression therapy, which depending on if they have an ulcer or not is gonna vary. Compression therapy can include stockings to start with typically. But also, if stockings aren't working as well, there are devices, portable devices for example, that can be utilized. There are other types of wrapping and bandaging that can be utilized. I think it'll be determined a little bit by the local practitioner's expertise, but additional compression adjuncts are allowed.
In terms of medical therapy, we'll make sure that the study teams review the history of DVT and make sure that the people who really do merit extended anti-coagulant therapy are getting that extended anti-coagulant therapy. There are also venoactive medications. There's a venoactive medical food approved by the FDA that can be utilized. For some people, Pentoxifylline can be utilized. Then, people who have venous ulcers are required to be managed in a professional wound care clinic. It's not just something that the doctor's doing in the office, but something that really gets that expertise. So, that's what everyone is getting.
In addition, half of the patients will be randomized to receive endovascular therapy that will consist of iliac vein stent placement, followed by a reassessment at two to four weeks to see if they're still symptomatic and if they have saphenous reflux. If they're still symptomatic, and they have saphenous reflux, then that can be ablated using intravenous techniques.
Steve: What is the anatomy that you don't want? What are some of the exclusion criteria?
Suresh: All the patients are required to have a baseline ultrasound. If there is poor inflow to the common femoral vein, then they would be excluded from this study. In terms of the IVC, the only thing that would exclude them is if they have obstruction of an IVC filter that's in there, mainly because the complexity and the variability around how you deal with that filter could be quite enormous. But even if they have an IVC obstruction or narrowing, and there's no filter, they can still be included.
Steve: So, it's not just stenting of the iliac, it's that you're stenting the disease from the inguinal ligament up?
Suresh: Yes, if it goes into the common femoral vein, we would recommend extending the stents.
Steve: Right. You have to do that. Now as an aside, this is the question that we're all wrestling with at this point, especially when we're doing studies, is what constitutes good inflow and lousy inflow? All of us say when I see it I know it, but is there a guideline given to the people in the trial?
Suresh: There's guidance, but not necessarily prescriptive sort of specifics. What we've said is that really we would expect there to be one excellent, deep tributary vein into the common femoral vein. Meaning the femoral vein, or the profunda, should be a good-looking vein. If it's the profunda, 9-10 millimeters. You know, a decent looking vein. If either of those doesn't exist, then we would say don't enroll the patient.
Steve: How about the treatment itself? If someone is randomized to endovascular intervention, how standardized is that, regarding the type of stent? If someone's randomized endovascular, what are they getting?
Suresh: The current devices are off-label. We're doing this with an IDE from the FDA. What they're allowed to use is self-expandable stents made of Elgiloy or Nitinol of at least 12 millimeters diameter. That gives them the choice, you know?
Steve: It's politically correct, I would say.
Suresh: Yes. I'll mention too, though, if we get approvals of venous stents this year, which hopefully we will, we will be allowing and encouraging their use in the study.
Steve: And you wanted them to stent, obviously, the entire disease going from a common femoral all the way up to the IVC?
Suresh: Absolutely. We've required that they pre-dilate the venous segment well and that they stent and dilate it well as well because we know that under-stenting is just gonna lead to a problem in the long run. What we've said in the protocol is that, for the most part, we think most people will get 14's or above. However, sometimes 12 does make sense once in a while, yeah.
Steve: If this is really a narrowed segment, and you just can't get it open, I agree. So now you've put the stent in and what's going on? What's a patient doing post-procedure?
Suresh: What we've said is that people who are randomized to endovascular therapy need to get anticoagulation for the six months afterward. We've strongly recommended that it be Lovenox for the first one to three months and then transition to an agent that we would like to be twice daily, in addition to aspirin as well.
Steve: Okay. You and I, we're into the minutia, but not everybody listening or reading this may be into the minutia. So, explain to them why you are recommending Lovenox or Enoxaparin for the first month or three months versus some DOAC or something else?
Suresh: Well, we know that the occurrence of stent occlusions is gonna be more likely early on, because we traumatize the venous system. And we know that in the post-thrombotic syndrome population, specifically, these are clotters. The rates of stent occlusion are substantial overall in the history that's been presented so far. We think we need to be on the more aggressive end of things.
Coumadin, unfortunately, the levels go up and down. And during that immediate post-procedure period re-occlusions can be frequent. Rivaroxaban, in the experience of some people - and again there's no comparative studies here - but in the experience of many of us a once daily agent like Rivaroxaban hasn't been that effective in doing that much better. We think a twice-daily agent might be better. For example, Apixaban. However, there's just not enough experience to know that yet. In our experience with Lovenox, while it's certainly not the most convenient or inexpensive drug to provide, just from a standpoint of saying, "well, we feel like we did the best we could", it's our feeling that right now that's probably the best choice.
We're recommending that it be started before the procedure. In other words, what we don't want is in the three days after the procedure messing around trying to get the drug, you know? We want them to really, ideally, start it before. Then, it can just be continued through the procedure period. Ultimately, eventually, we anticipate that most patients will transition to an oral agent.
Steve: That's what most of us are doing already. It's very important to start it beforehand, not just to get the level of the drug, but so that the patient feels comfortable. Like you say, that first day or two afterward, patients are overwhelmed and say, "how do I do this?" So, are you mandating at least a month? Or, are you suggesting?
Suresh: For Lovenox, we strongly recommend. And part of that, remember, is that we can't control the insurance situation. We would have mandated it, except that can be a burden, a cost burden on patients.
Details of participation
Steve: So, there's no money within the grant for this to be paid for the patient?
Suresh: Correct.
Steve: If you believe strongly, as I do in the Lovenox, you'll want to make sure patients are going to be able to qualify before you enroll them.
Suresh: What the study does is we have what we call a run-in period. Patients first meet the eligibility criteria before they're entered into what we call a run-in period of at least three weeks, where they all get provided the basic standard of care. The idea is that some people may never have even tried compression therapy at all. During that time period, we do a pre-certification with their insurance.
Steve: Perfect. How long is the study going for?
Suresh: Two years.
Steve: Does this mean the patients who are randomized to non-intervention cannot be intervened on for two years?
Suresh: The study protocol would strongly discourage it; however, we realize that you can get into situations where the patient is absolutely insisting on something, and where you cross an ethical boundary a little bit, right? There is the potential for some people to cross over if needed. We certainly don't encourage it from a study perspective, but we realize that that is something we may have to contend with. Certainly, with this population, it's likely that we may have to contend with it.
Endpoints
Steve: All right. Talk to us a little bit about the endpoints that you're measuring.
Suresh: Yeah. The primary endpoint is the Venous Clinical Severity Score at six months after randomization, adjusted for the baseline score. Basically, it's the change, in essence, in the severity of their venous disease. We're also assessing the Villalta scale as a secondary measure of post-thrombotic syndrome. We're also assessing health-related quality of life, using both venous disease-specific and general health-related quality of life measures. We're also assessing and measuring the venous ulcers that people have and are reporting out the percent that the wound healed and how many healed completely within 24 weeks. We're also reporting safety issues and occurrences of recurrent venous thromboembolism, major bleeding, and anything else. We're also doing a health economics study as part of this over the two years.
Steve: That's a lot of stuff measured. Now, one thing you didn't mention, and I agree with you, it's not a primary or secondary endpoint to whatever it is. When and how are you assessing stent patency in those people who receive a stent?
Suresh: We're assessing it with ultrasound at six months. Again, we're doing ultrasound assessments in all patients in the study at six months and at baseline. In terms of any more invasive assessment, we're not doing anything invasive during follow-up. In that sense, this is very different than, for example, a study that's aimed at getting a stent approved by the FDA, for example, where you're really focused on the device. We're really focused more on health outcomes, the two treatment strategies, of which stenting is part of one of the strategies.
Steve: Yeah. No. I agree with you. I think we're all moving to that when we're talking about studies like this, as you said, aside from trying to get the device or a stent approved. I think quality of life is the thing. You're only assessing stent patency at six months, so nothing prior to that? Is this correct? You're not imaging the stent prior to that?
Suresh: Correct.
Steve: Okay. I'll go back a little bit. One of the concerns with the ATTRACT trial was the assessment of the disease and the assessment of the efficacy of the stents, stenting the full disease, et cetera. Some people felt more IVUS should be have used—intravascular ultrasound. Are you assuming everyone who is putting a stent in is going to be using intravascular ultrasound too?
Suresh: We require sites, after the stents are placed, to use IVUS. Before the stents are placed, they're strongly encouraged to use IVUS, but it depends. Sometimes it's more important than other times, but certainly, after they've placed them we want them to use IVUS and look and make sure things look good.
Steve: I agree with you. 'Cause many times, pre-stenting, you kinda know this whole disease. You don't need the IVUS to say this patient has occlusal disease or not, but certainly, post I agree. You wanna make sure that the stent is as open as it can be.
Suresh: Yep. Absolutely.
Hope for patients with post-thrombotic syndrome (PTS)
Steve: All right. You go into two years and what do you hope to find? I'm not asking you to predict. If you had your druthers ...
Suresh: What we want most of all is whatever it is that we find to represent what actually occurs. But having said that, it would be delightful if the study validated a new option that is able to actually reduce disability in this population, right? So if we found that the Venous Clinical Severity Scores were better, that health-related quality of life was better, that ulcers heal faster—which is complicated. It may or may not occur, we don't know—and also that the results were sort of sustained, time-wise. We anticipate a relatively low frequency of complications with this particular treatment, but I think that really it's the efficacy. That is determined partly by the stent patency as well, obviously, over the first two years right? I think that if we find that the people are doing better at two years in their Venous Clinical Severity Scores and quality of life, then I think we've really achieved something in terms of providing a strong foundation to advance care in a particular way.
Steve: I agree with you. Many of our biases are that placing the stent in the right patient does improve their quality of life. That's our bias, but that's why you're doing the study, and I think it's great. I think you learned a few things from the ATTRACT trial. It's a more narrow, uniform-type of study. As you say, you're addressing a disease that can be quantified a little bit more. I mean, you know it when it's there. You're only dealing with from the inguinal ligament on up, which I think is good as well. It will help us a lot. Anything else you wanna say to those listening or the public about the trial or anything?
Suresh: Well, I think it's a great opportunity, and even the ATTRACT results point in the direction that this may be a great opportunity. We just published the iliofemoral DVT subgroup paper for the ATTRACT trial in Circulation in December. That trial found that even with iliofemoral DVT, lysing people up front doesn't prevent PTS, but it does reduce the severity of PTS. It improves their quality of life more than standard therapy does. With that in mind, the idea that having an open iliac vein is important to patient's quality of life is something that we're now assessing in a different context here. I think that were this trial, for example, to be positive, then I think the next step would be: okay, we really need to make providers aware of this idea that an iliac vein needs to be kept open. And, again, we need to develop that evidence, but I think that would be a very exciting advance in care if it were to happen that way.
Steve: Well, I think you're right, and I think it's great. You brought out all the points about the trial, and now let's hope that this will also add to people submitting patients for the trial.


