Lipedema is a genetically transmitted, loose connective tissue disease of subcutaneous fat tissue. There are many differences in the subcutaneous tissue in women with lipedema compared to women without lipedema; these include increased sodium content, increased tissue edema, adipose tissue hypertrophy, increased cellular inflammation, microvascular dilation, and different gene expression.1 While these differences are becoming more known, what is often focused on, especially by the media, is abnormal adipose tissue, more colloquially known as “abnormal fat.”
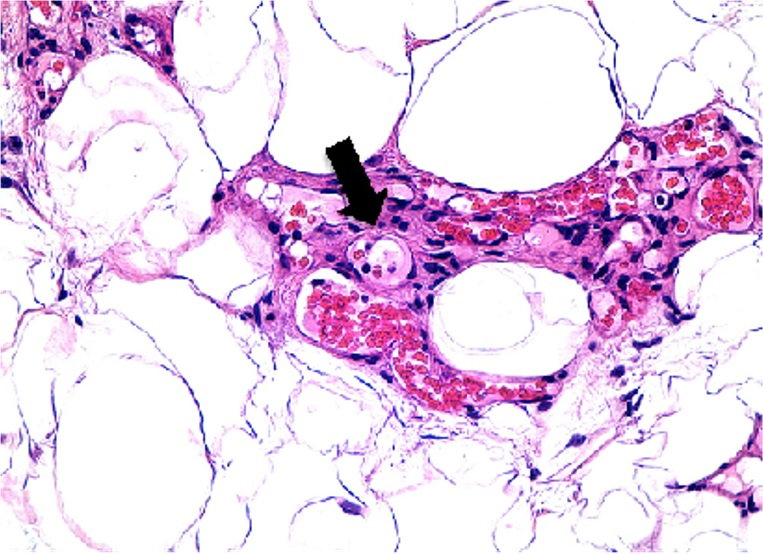
Angiogenesis in Non-Obese Lipedema leg fat. H&E stain. Arrows indicate blood vessel lumens embedded in connective tissue around adipocytes.1
How Is Lipedema Fat and Metabolism Different?
Compared to body mass index (BMI) matched controls, individuals with lipedema are more insulin sensitive as measured by glucose tolerance tests (GTT) and euglycemic insulin clamp glucose sensitivity. Fat in the distribution of lipedema is called gynoid fat and is considered cardio-protective when compared with the central android fat of lifestyle-induced obesity.

Sam Klein, M.D. Washington University, School of Medicine. St Louis, Missouri
Lipedema fat is relatively resistant to weight loss. Women with lipedema have a greater percentage of body fat compared to BMI-matched controls. With 10% body weight loss, the percentage of body fat does not change significantly when measured by dual absorption x-ray (Dexa).
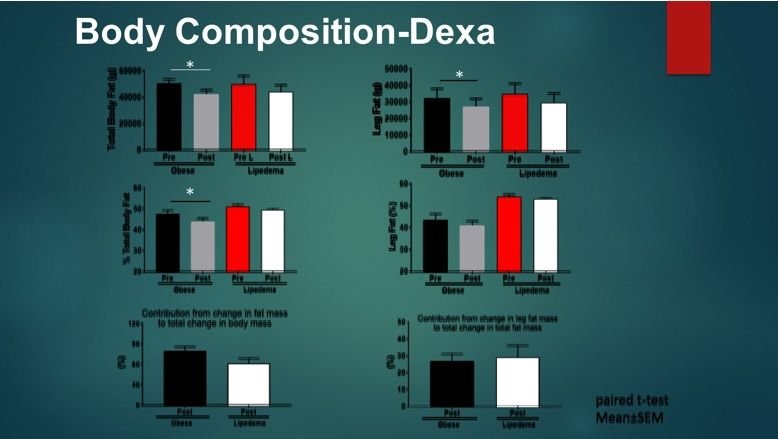
Sam Klein, MD. Washington University, School of Medicine. St. Louis, Missouri.
Why is Lipedema Fat Different?
It is not fully understood why lipedema fat is more resistant to weight loss; however, other diseases can give researchers important clues. It is known that lifestyle-induced obesity can result in the growth of fibrotic, subcutaneous adipose tissue that reduces the ability to lose weight after bariatric surgery. Tissue affected by lymphedema can also undergo a fatty fibrotic transformation. In the cases of prolonged lymphedema, chronic interstitial fluid accumulation leads to both subcutaneous tissue fibrosis and adipose deposition, often resulting in massive hypertrophy of the affected area. The longer lymphedema persists and the more poorly it is managed, the greater the risk of developing significant excess adipose tissue deposition complicated by fibrosis becomes.2
Lipedema is seen almost exclusively in women, and it often progresses during times of hormonal change. Does estrogen or progesterone trigger a change in the adipose tissue of women with lipedema? A mutation in the Aldo-Keto Reductase 1C1 (AKR1C1) gene was found with lipedema that makes this enzyme less efficient in reducing progesterone to hydroxyprogesterone, which could drive increased subcutaneous fat deposition. These are all clues but are not a comprehensive picture of the etiology of lipedema.

Cross-sections of a lymphedematous (right) and a normal arm (left) showing abundance of excess adipose tissue in the affected arm.3
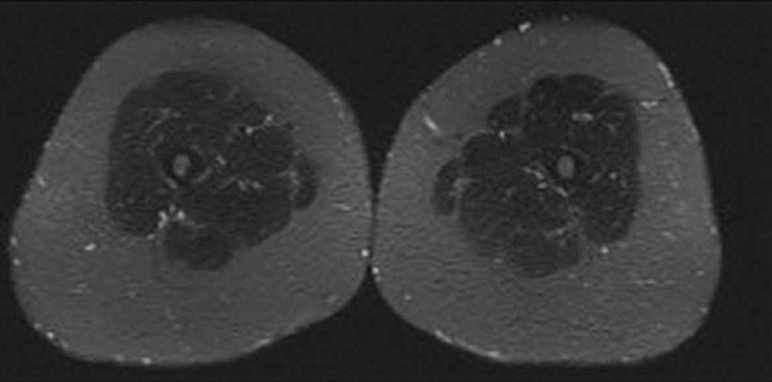
Bilateral Symmetric Fat Hypertrophy in Lower Leg on Woman with Lipedema as shown by MRI cross-sectional Images. Image Provided by Thomas Wright.
What Is BMI and Why Is It an Inaccurate and Potentially Misleading Description of Lipedema and Other Diseases?
Body Mass Index (BMI) = weight in kilograms divided by height in meters squared. BMI is simply an overall numerical score (like height and weight from which it is derived) that is not a biological representation of a person’s overall health.
Interestingly, this formula was not originally used for individual health assessments at all! While BMI has been around since the early 19th century, the man who initially created the calculation knew at that time that it was flawed. Lambert Adolphe Jacques Quetelet, a Belgian mathematician, created the BMI formula as a way to quickly and easily estimate what percentage of the overall population might be obese. He was attempting to assist the country’s leaders in properly allocating resources in the 1830s. The formula Quetelet produced is not biologically valid or based on any metabolic or physiologic principles. In other words, it is a 200-year-old hack that was never intended to describe or diagnose obesity.
Obesity is defined by the World Health Organization (WHO) as having a BMI at or above 30 kg/m².4 Lipedema, which can lead to an increased BMI, is often confused with non-lipedema obesity. As explained above, the excess subcutaneous adipose tissue that occurs in lipedema has different metabolic effects than the central fat accumulation of obesity, but both obesity and lipedema are associated with an increased BMI. Using only BMI to define obesity can be inaccurate because it can represent two very different disease states, i.e., insulin sensitivity and a gynoid location of fat in lipedema, and insulin resistance and android or abdominal location of fat in lifestyle-induced obesity.
Increased BMI due to increased muscle mass, especially in athletes and bodybuilders, can signify a healthy individual, and it is not associated with the same risks as central obesity. Muscle mass has a higher density than fat, and therefore, has a larger impact on BMI. A female bodybuilder may have a higher BMI than average, but diagnosing her as obese would be inaccurate. Similarly, Lipedema causes higher BMI, but this will not correlate with higher cardiovascular or diabetes risks.
Waist-To-Hip Ratio
What can be used instead of BMI to better assess cardiovascular risk? A few studies show that waist-to-hip ratio (WHR), at least in women, is a better marker for cardiovascular disease risk than BMI.5 However, just measuring waist circumference instead of waist-to-hip ratio is the same as using BMI to predict the risk of cardiovascular disease. During the COVID-19 pandemic, it may be difficult to get close enough to patients to measure circumferences. New mobile applications have been developed that can take photos of patients and calculate circumferences. As such, these new applications may be the future of measuring cardiovascular risk.
Adipocytes of Lipedema
Do the adipocytes of lipedema and obesity have a different biology and physiology, or are they bystanders in their environment? In other words, do the fibrosis and lymphatic changes seen in lipedema change the fat cell? Are these changes triggered by hormones or are they triggered by some other cause? As more is learned about lipedema, a better understanding of adipose biology is gained, helping to better understand some of the most prevalent diseases of our time.
How BMI of 30kg/m2 Looks

Woman with lifestyle-induced obesity and BMI of 33

Person with type 3, stage 2 lipedema who has a BMI of 30

Female bodybuilder with BMI of 30
References
- Al-Ghadban, Sara, Walter Cromer, Marisol Allen, Christopher Ussery, Michael Badowski, David Harris, Karen L. Herbst. "Dilated Blood and Lymphatic Microvessels, Angiogenesis, Increased Macrophages, and Adipocyte Hypertrophy in Lipedema Thigh Skin and Fat Tissue." Journal of Obesity, vol. 2019, Article ID 8747461, 2019. https://doi.org/10.1155/2019/8747461.
- Mehrara, B. J., A. K. Greene. “Lymphedema and Obesity: Is There a Link?.” Plast Reconstr Surg. 2014;134(1):154e-160e. doi:10.1097/PRS.0000000000000268.
- Borson, Hakan, Carolin Freccero. “Liposuction as a Treatment for Lymphoedema.” https://www.eurolymphology.org/wp-content/uploads/2011/01/5-page-11-25-Brorson-proof-10.pdf.
- World Health Organization G. “Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation.” Geneva: 2000.
- Rudolf E Noble, R. E. "Waist-to-hip ratio versus BMI as predictors of cardiac risk in obese adult women" PMID:11290672