
As pneumatic compression therapy becomes more sophisticated, it is growing in scope of influence as a powerful tool to treat a multitude of circulatory conditions, heal post-op patients and help amputees. This technology is also heavily relied on by world class athletes and sports organizations looking to optimize their performance. Dynamic intermittent compression is recommended for increasing the healing rate of wounds, especially in the presence of severe venous stasis ulceration, venous insufficiency or chronic non-healing wounds. Pneumatic compression is typically employed as a continuum of care treatment, secondary to, and in conjunction with, conventional methods. Regular use is also associated with a decrease in the rate of ulcer recurrence.1 Advanced pneumatic compression devices are able to enhance venous and lymphatic return, improve circulation and reduce swelling and tissue pressure.2
Physicians who treat circulatory conditions all too often encounter patients with wounds that stubbornly persist for months, if not years—wounds that often worsen despite time-consuming and expensive treatments. Modern wound care frequently focuses on the importance of optimizing the wound microenvironment by addressing infection, debriding necrotic tissue, and through advanced dressings, topical treatments and growth factors. However, patients with non-healing wounds often suffer from clinically significant underlying circulatory compromise caused by arterial, venous or lymphatic insufficiency, creating further impairment to efficient healing. Additionally, such patients also exhibit high tissue pressure in the area around wounds due to indolent cellulitis, lymphatic engorgement, induration, fibrosis or edema. Dynamic compression therapy addresses underlying circulatory issues by enhancing venous and lymphatic return, leading to reduced tissue pressure at wound sites.2,3 Doctors are increasingly advocating for the use of pneumatic compression devices as part of treatment plans in such cases.
The late Laura F. Jacobs, MD, PhD, FAPWCA, a pioneer in venous abnormalities and pneumatic compression therapy, dedicated her career to improving treatment options for patients with non-healing wounds who did not respond to traditional regimens. Specifically, in her efforts to treat such patients, Dr. Jacobs began addressing the underlying circulatory disorders with pneumatic compression devices (PCDs). This ultimately led to a career-long endeavor to improve pneumatic compression, and to achieve profound healing results for her patients. Her work also led to the development of the NormaTec PCD, a highly sophisticated dynamic compression device. The NormaTec PCD uses biomimicry to enhance circulation through a patented sequence of pulsing, gradients and distal release. The device mobilizes fluid and increases blood flow to the limbs through a pulsing action that is designed to simulate the muscle pump of the legs. NormaTec’s patented PULSE Technology also uses hold pressures to work synchronously with the one-way valves of the veins and lymphatic vessels, preventing fluids from moving in the wrong direction.
In response to patients’ successes and continued dedication to innovation, in February of 2017 NormaTec introduced the Via and Via Elite Pneumatic Compression Devices to the medical community. Weighing only 3.2 pounds, the devices are significantly lighter and more portable than other pneumatic compression devices. The settings are highly customizable to tailor treatment area and pressure to individual patient needs, and all controls are intuitive and digital, making them simple for patients to use. The NormaTec Via Elite also includes a built-in compliance monitor that positively influences patient compliance while also allowing physicians to audit use. These advancements, coupled with the patented PULSE Technology and multicompartmental gradient pressure design of NormaTec’s attachments, are redefining the capabilities and the relative ease of use of pneumatic compression therapy.
Patient experience using pneumatic compression therapy varies relative to the conditions being treated. Patients with acquired or congenital lymphedema and those with chronic venous insufficiency utilize the technology daily to manage their symptoms as well as prevent the development of progressive conditions such as deep vein thrombosis and cellulitis. Lymphedema and cellulitis can often be a vicious cycle, and regular use of dynamic compression therapy can prevent the reoccurrence of cellulitis.4 Such patients are advised to utilize pneumatic compression therapy for 15-20 minutes twice per day at the lowest setting, and then gradually increase usage up to one hour in one or two sessions per day. Pressure can be increased slowly as tolerated, but patients should always keep the pressure to a comfortable level. Patients who have previously tried compression garments, manual lymph drainage and elevation techniques without seeing positive outcomes, as well as those who are unable to don compression garments due to size restrictions, have seen great success with pneumatic compression therapy.5
PCT for Wound Healing and Professional Sports
Patients attempting to heal wounds, both chronic and those related to surgery, are seeing decreased healing times thanks to the advantages of pneumatic compression therapy.5 Patients are advised to utilize dynamic compression therapy at frequent intervals to start, and then to taper treatment sessions until they are pumping only one or two times per day. Unlike lymphedema and CVI patients, post-op and chronic wound patients should eventually be able to discontinue use. Pneumatic compression devices contribute to a reduction in post-op swelling,6 enhanced circulation, vigorous healing rates and also help with pain management, leading to improved mobility and rapid recovery times.7
Wound Healing—The patient is a 75 year-old male with bilateral lower extremity venous insufficiency with lymphedema and multiple ulcerations. His past medical history includes MI, CABGx4, DM, obesity, and multiple episodes of cellulitis requiring oral and IV antibiotics. His symptoms were present for many years, and he previously tried elevation, exercise, compression bandaging systems, diuretics, wound dressings and participation in a wound care center.

Left: Chronic non-healing wound with significant edema and active cellulitis.
Right: After 10 days of at-home NormaTec pneumatic compression therapy.
Lymphedema Management—The patient is a 74 year-old male with bilateral lower extremity venous insufficiency and lymphedema with ulcerations. His past medical history includes multiple episodes of cellulitis, A-Fib, DM, Diabetic Peripheral Neuropathy, DJD, GERD, HTN and PVD. His symptoms have been present for several years. Previously, he tried elevation, exercise, wound dressings, debridement, gradient compression garments, bandaging, antibiotics and participation in a formal wound care program.
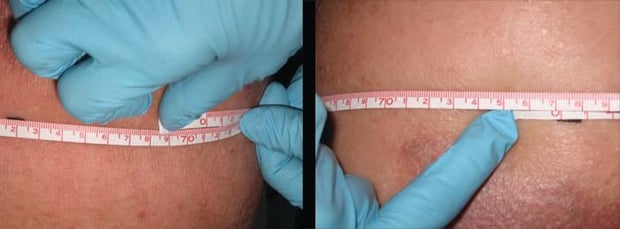
Left: Lower extremity lymphedema—initial calf measurement of 77 cm.
Right: After 15 minutes of treatment with NormaTec pneumatic compression therapy—decreased by 6 cm.
Physicians are also utilizing pneumatic compression therapy with amputee patients to facilitate a host of benefits. Enhanced circulation to the residual limb speeds up healing times for skin problems and wounds. Additionally, patients report relief from neuropathic and residual leg pain, a frequent issue for amputees. The treatment also helps to reduce swelling and inflammation to the area, leading to increased mobility and a more consistent, proper fit for prosthetic attachments.
While clinicians were successfully treating venous insufficiency, complex wounds and post-operative complications with pneumatic compression, the sports world began to realize a unique set of benefits from the technology. Compression garments have long been used by athletes to increase circulation and prevent inflammation and edema. The dynamic compression and patented massage sequence of the NormaTec was found to enhance natural recovery time and to give athletes a competitive edge when training and competing in demanding schedules.8
Growing Demand, Evolving Products
In response to growing demand, NormaTec developed the PULSE and PULSE PRO to cater specifically to the needs of athletes and the professionals who treat them. The sports medicine devices are sought out for rapid athlete recovery and rehab between intense training and competition. NormaTec’s patented dynamic massage sequence, customized pressures and specialized design yield exceptional recovery times for athletes, who also see relief from sore muscles and inflammation, experience expanded range of motion and have an increased pressure to pain threshold.9,10 The technology is now used extensively by pro athletes and therapists in the US military and in professional sports, as well as by serious amateur athletes in sports like running, triathlon, functional fitness, golf and beyond. Wide adoption of NormaTec’s technology has been part of a profound shift in athletics, with recovery being recognized as an increasingly integral part of success.
As professional teams increased their usage of NormaTec Recovery Systems, most notably the NormaTec PULSE PRO, which is also used as a rehab modality, they began creating dedicated recovery rooms in their training facilities. Today many Olympic training facilities, such as the USTA Player Development center in Florida, and major team facilities such the Baltimore Ravens Under Armour Training facility, the Brooklyn Nets Barclays Center, the Philadelphia Flyers Skate Zone, and many other high-profile teams, prestigious institutes and official facilities have been modified to include NormaTec Recovery Rooms for their athletes.
Dynamic pneumatic compression technology applications continue to evolve within both the medical and sports worlds. Physicians treating patients affected by a diverse number of acquired, acute, chronic and congenital circulatory conditions are realizing the benefits of PCDs as part of their treatment regimen. Athletes are also utilizing the technology to increase human performance and to harness the significant recovery benefits of NormaTec’s PULSE technology. Recent advancements to devices like the NormaTec Via and Via Elite are increasing ease of use for patients, enhancing compliance and ultimately improving patient outcomes. With such an impressive roster of capabilities and far reaching influence in medicine, as well as widespread adoption among athletes, pneumatic compression is emerging as an essential tool for the modern physician.
References
- Comerota AJ. 2011. “Intermittent pneumatic compression: physiologic and clinical basis to improve management of venous leg ulcers.” J Vasc Surg 53 (4):1121-9.
- Adams KE, Rasmussen JC, Darne C, et al. 2010. “Direct evidence of lymphatic function improvement after advanced pneumatic compression device treatment of lymphedema.” Biomed Opt Express 1 (1):114-125.
- Laura Jacobs MD, PhD, FAPWCA. 2006. “Pneumatic Medicine and Rapid Would Healing.” APWCA Winter.
- Karaca-mandic P, Hirsch AT, Rockson SG, Ridner SH. 2015. “The Cutaneous, Net Clinical, and Health Economic Benefits of Advanced Pneumatic Compression Devices in Patients With Lymphedema.” JAMA Dermatol 151 (11):1187-93.
- Smith PC, Sarin S, Hasty J, Scurr JH. 1990. “Sequential gradient pneumatic compression enhances venous ulcer healing: a randomized trial.” Surgery 108 (5):871-5.
- Westrich GH, Sculco TP. 1996. “Prophylaxis against deep venous thrombosis after total knee arthroplasty. Pneumatic plantar compression and aspirin compared with aspirin alone.” J Bone Joint Surg Am 78 (6):826-34.
- Talbot SG, Kerstein D, Jacobs LF, Upton J. 2012. “CASE REPORT Postoperative Use of the NormaTec Pneumatic Compression Device in Vascular Anomalies.” Eplasty 12:e6.
- Hanson E, Stetter K, Li R, Thomas A. 2013. “An Intermittent Pneumatic Compression Device Reduces Blood Lactate Concentrations More Effectively Than Passive Recovery after Wingate Testing.” J Athl Enhancement 2:3.
- Sands WA, McNeal JR, Murray SR, Stone MH. 2015. “Dynamic Compression Enhances Pressure-to-Pain Threshold in Elite Athlete Recovery: Exploratory Study.” J Strength Cond Res 29 (5):1263-72.
- Sands WA, Murray MB, Murray SR, et al. 2014. “Peristaltic pulse dynamic compression of the lower extremity enhances flexibility.” J Strength Cond Res 28 (4):1058-64.


