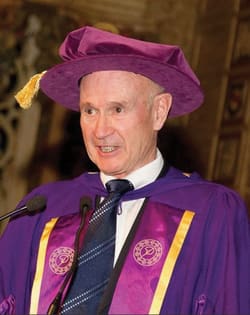
Dr. Mitchel Goldman, Volunteer Clinical Professor of Dermatology/Medicine University of California, San Diego and Medical Director of West Dermatology, sits down with his favorite mentor–the legendary, Dr. Hugo Partsch.
 Dr. Mitchel Goldman: You are one of the most significant mentors that I’ve had in my phlebology career. There are so many important people that I have interacted with in phlebology, from the very first person Arnost Fronek, Anton Butie and David Duffy through our French colleagues, JJ Guex, Frederik Vin, Michel Shadeck, Claude Guard and Andre Cornu-Thenard and our Italian colleagues, especially Leonardo Corcos, Stefano Ricci and Michael Georgiev, and colleagues in the Netherlands, especially Martino Neumann. For some reason my interaction and friendship with you has always stood out as being perhaps the most significant of my phlebological career. I don’t know why! It just is.
Dr. Mitchel Goldman: You are one of the most significant mentors that I’ve had in my phlebology career. There are so many important people that I have interacted with in phlebology, from the very first person Arnost Fronek, Anton Butie and David Duffy through our French colleagues, JJ Guex, Frederik Vin, Michel Shadeck, Claude Guard and Andre Cornu-Thenard and our Italian colleagues, especially Leonardo Corcos, Stefano Ricci and Michael Georgiev, and colleagues in the Netherlands, especially Martino Neumann. For some reason my interaction and friendship with you has always stood out as being perhaps the most significant of my phlebological career. I don’t know why! It just is.
Dr. Hugo Partsch: That’s very kind of you.
MG: My first question is could you briefly take us through your phlebological career, starting from the Medical University of Vienna?

HP: I was finishing my medical studies 1962, a long time ago, and then I was in a hospital close to Vienna where I started to work as a general practitioner. Then I moved to Vienna, where I started my dermatological training. Phlebology came into my direction when I met our nuclear medical person Dr. Adolf Mostbeck (and Dr. Helmut Haid from Germany) who wanted to demonstrate the efficacy of leg bandaging--the so-called Fischer bandage. Dr. Heinrich Fischer was a pupil of Dr. Paul G. Unna, the one who invented the zinc paste “Unna Boot” that is used so commonly in dermatologic treatment of leg ulcers.
Fischer used this bandage on people with deep vein thrombosis, and was surprised to see the immediate pain relieving effect it had. Dr. Haid, the grandson-in-law of Fischer, came to our department in Vienna to evaluate lymphatic transport under this bandage. We started to investigate lymphatic transport using lymphoscintigraphy in leg ulcer patients because this condition was very frequent at that time in our department. We began our studies investigating subfascial lymph transport and found that most post-thrombotic syndrome patients had highly diminished subfascial lymph transport.

When we used this bandage, lymph transport increased dramatically. This was the first publication I was involved in, and this was 1968. Since then, I became more and more interested, especially regarding the influence of compression also on deep vein thrombosis and other phlebological and lymphological conditions.
MG: What I find most interesting Hugo is how you turned the practical use of bandages into a true scientific study. When I look at your career and the hundreds of papers and book chapters that you’ve published, what comes to my mind is that you have turned what appears to be the obvious into a scientifically-validated study. That’s what really impressed me with your work in phlebology – the ability to apply scientific reasoning to what appears on the outside to just be some very practical types of treatments.
HP: You’re right. Since then, I’ve always tried to find out the mechanisms of action for different kinds of compression, and to use them in everyday practice to see the difference between elastic stockings and bandages and so on. We used several methods in our patients to investigate these effects, first starting with Doppler ultrasonography, plethysmography, venous pressure measurements, lymphoscintigraphy and indirect lymphography, and later Duplex and MRI in standing position. Everything was an attempt to clarify the mechanisms of action of compression.
MG: What I find fascinating is that it translates into the improvement of patient care. Of course you have always been incredibly modest, but some of the most important discoveries and proven hypotheses that at least I believe that you’ve proven is the treatment of deep vein thrombosis through the use of graduated compression and ambulation. I think this modernized the treatment of deep vein thrombosis, as well as your work on graduated compression and ambulation, and not only with sclerotherapy treatment for varicose veins but also endovascular techniques.
HP: You’re right--walking exercises with compression bandages in acute deep vein thrombosis was probably one of my most important practical recommendations. We did a randomized controlled study. We didn’t find enough patients of course, but anyhow we were able to show that bed rest can be detrimental for mobile patients by doing series of lung scans. We also showed that the patients may benefit from ambulation and compression in the acute stage of deep vein thrombosis concerning faster relief of pain and swelling. You’re right, this was probably my most important contribution.
MG: It certainly has been, and I think has improved the lives of countless patients throughout the world.
HP: Bed rest can be a dangerous treatment modality, especially with the elderly. Just recently I received an email from a nurse in South Korea--she was surprised by my recommendation that DVT patients need to be ambulatory. She was surprised that people with deep vein thrombosis don’t need to have bed rest. She says that in her country, all the patients are put into bed, and I believe this is the case not only in South Korea. Even in Western countries, many people are put into bed with deep vein thrombosis, including those who come in walking.
MG: Hugo, with this in mind, you have been instrumental in improving phlebological treatment not only in Austria and Europe, but throughout the world. This led to you becoming President of the International Union of Phlebology. Could you tell us something about your role as President of the International Union of Phlebology?
 HP: I was elected to be the President of the IUP in 1999 and I served for four years. I was nominated by Dr. Robert Stemmer. Dr. Stemmer was a famous colleague in Strasbourg, who had organized a spectacular World Meeting of the IUP in his town in 1989. As you know, we all are standing on the shoulders of previous great people. And one of these was Dr. Stemmer. In my case, he was the one who proposed me, and I was elected because at that time there was no other candidate. Can you believe that? This was 1989 at the IUP world meeting in Sydney.
HP: I was elected to be the President of the IUP in 1999 and I served for four years. I was nominated by Dr. Robert Stemmer. Dr. Stemmer was a famous colleague in Strasbourg, who had organized a spectacular World Meeting of the IUP in his town in 1989. As you know, we all are standing on the shoulders of previous great people. And one of these was Dr. Stemmer. In my case, he was the one who proposed me, and I was elected because at that time there was no other candidate. Can you believe that? This was 1989 at the IUP world meeting in Sydney.
Promoted by Leonel Villavicencio, Norman Rich and Leo Widmer, I organized the Fifth European American Symposium on Venous Diseases in Vienna at which George Feagan turned up again from his African exile, freezing in the November cold.
My main intention during my IUP presidency was to initiate internationally-accepted consensus documents. It’s nowadays routine practice for the IUP to come out with consensus papers, but at that time this was new. We started with anatomical nomenclature, compression and with two papers on how to investigate a patient using duplex. So these were the first consensus papers coming from the IUP.
“I find it is most exciting if you understand something that has not been understood before. If you know this feeling, you want to share this it with others, and tell them your insight on this subject. This seems to me to be the driving force of education.”
MG: Also of equal importance were the revised classifications of venous insufficiency. Could you share your role in developing the CEAP classification?
HP: I was involved in this conference in Hawaii together with Bo Eklof and Andrew Nicolaides, who were the motors of the CEAP classification team. Including the “History” of the patient, some had proposed to term it the “CHEAP” system.
MG: Yes. What other highlights do you recall from your presidency in the IUP?
HP: There were not many highlights I must say. There were a lot of political struggles with different countries claiming not one society but many societies should represent a country, so at the end I opened it up to multiple societies from each country and maybe made things even worse.
MG: Yes, but I think that you sell yourself short, because one of the qualities that I believe that you possess is the ability to make people more comfortable, and you tried to establish a better order in the IUP. Because you were able to listen to multiple sides and present a very good resolution, I think that you did not upset most of our members as they would have been. You were a very successful president.
HP: That’s very kind of you. I tried to serve mainly and not put myself in the first row.
MG: Hugo, one of the things that you said a little while back is that “most of us are always standing on the shoulders of those that preceded us,” and you mentioned that one of your great mentors was Dr. Stemmer. Are there any other mentors that you would like to acknowledge at this time?
HP: Maybe there’s Dr. Robert May, who discovered the May-Thurner Syndrome with Dr. Josef Thurner. Dr. May was one of the greatest venous surgeons in Austria. I had to organize the first conference on perforator veins together with Dr. May, which was in 1979. There was even a book coming out, and all the discussions since then you may find already in this book from 1979. For instance, the idea that “blow-down” is obviously more important than “blow-out” and all the recent discussions. There were Drs. Frank Cockett, Raul Bjordal and Olav Thulesius with us in this meeting, and other famous colleagues.
Another shoulder I stood on was certainly Dr. Alfred Bollinger, an internist from Zurich, Switzerland, who died last year. Together, we published a book about initial lymphatics, in which we reported our findings with indirect lymphography as the first in the world in humans. The findings, using new water-soluble contrast media, fit well with his results of fluorescence microlymphography, so we came together and published a book on initial lymphatics.
This was 1984. Standing on the shoulders of Dr. Stemmer, we published a book on compression therapy in 2000. Actually, Dr. Stemmer did all the work, but he was kind enough to put my name and that of Dr. Eberhard Rabe in front of his name, just in alphabetical order.
“Phlebology has become more and more of a “varicology,” so people are interested mostly in treating varicose veins. My main interests as a hospital person were rather severe conditions like ulcers, deep vein thrombosis, lymphedema or angiodysplasias and vascular malformations.”
MG: One of the other qualities that I and so many of your friends and colleagues admire about you is your love for teaching. I think you’ve probably visited almost every country on this planet, and have touched perhaps even 100,000 phlebologists. What drives you to teach? What do you enjoy most about teaching?
HP: To share my experience and my knowledge with other people. For me, this is a kind of driving force, and I find it is most exciting if you understand something that has not been understood before. If you know this feeling, you want to share this with others, and tell them your insight on this subject. This seems to me to be the driving force of education.
MG: Is there any one of your teaching experiences that stands out most in your long career?
HP: Not as a single action, I would say. But trying to bring people together by sharing common interests was certainly one motive to create the International Compression Club (ICC) in 2005. It was meant as a platform for industry and for those few people who are really interested in compression.
MG: Do you have any advice for the younger phlebologists on how to live their life and advance the field of phlebology?
HP: Phlebology has grown tremendously in the past 50 years. I still remember the time when you were among the first presidents of the North American Society of Phlebology, now the American College of Phlebology.
Since then, the field has developed dramatically. Many new diagnostic and therapeutic methods were coming in. Phlebology has become more and more of a “varicology,” so people are interested mostly in treating varicose veins. My main interests as a hospital person were rather severe conditions like ulcers, deep vein thrombosis, lymphedema or angiodysplasias and vascular malformations. This isn’t as interesting to most modern phlebologists, and I understand that because it’s cumbersome and much harder to live from.
MG: Are there any last comments you’d like to make, Hugo?
HP: I hope that phlebology will go on, not only in the direction of “varicology,” but also through our colleagues’ initiatives to treat ulcers. At the moment, this task is given into the hands of wound healing centers that often prescribe local dressings without any understanding of the underlying pathology. Many of these are extremely expensive, and the prescribers forget that people with ulcers suffer from severe diseases that need to be first diagnosed correctly, which is rarely the case. Also, “purely venous” ulcers deserve an exact diagnosis by using at least a Duplex investigation and adequate treatment repairing venous drainage and not just wound dressings to improve local symptoms.
There was an initiative by the American Venous Forum some years ago to reduce the incidence of leg ulcers in the next 10 years by 50%. So I’m afraid that this goal will not be reached. There is also a social dimension because when our colleagues don’t treat these patients, they will go to inadequately trained caregivers to get relief for their problems.
MG: Hugo, thank you so much for taking the time to do this brief interview. I know that 30 minutes does not do justice, but I just want to let you know not only on my behalf but also from countless other phlebologists that we’re so grateful for you and your love for teaching, and for bringing phlebology into the modern world. I really appreciate the opportunity to interview you.
HP: You’re so kind to me, Mitch. When was it? When was the last time you visited Vienna, can you remember?
MG: We did our first symposium together in 1990 when I was Program Co-Chairman with you at the Venous European/American Symposium on Venous Diseases, and then in 1993 when we held a phlebology workshop. I had a wonderful time then, and every time I see you Hugo, I have a wonderful time and I learn something new.
HP: Very kind of you, thank you Mitch. Thank you so much.
MG: Okay, auf wiedersehen my friend.


