In 2002, Drs. S Raju and Peter Neglen reported their initial experience with diagnosing iliac vein stenosis.(1) They described that intravascular ultrasound (IVUS) could identify discrete segments of the common and external iliac veins (CEIV) that were narrowed due to compression of the vein by the adjacent artery or previous thrombus. Historically, this pathologic anatomy has been recognized, labeled May-Thurner Syndrome (MTS), and has a known association with extensive left leg iliofemoral deep vein thrombosis (DVT). Until recently, MTS was usually diagnosed with venography after thrombolysis of the acute DVT and treated with balloon angioplasty and stent. (2)
 Stenosis Discovery
Stenosis Discovery
Raju and Neglen further identified that many patients with advanced (CEAP 3-6) chronic venous disease (CVD) had stenosis of the iliac veins in the absence of acute DVT that appeared to be flow limiting. (3) A certain number of advanced cases of CVD in fact, have a non-thrombotic (primary or idiopathic) or post-thrombotic (secondary) cause. Iliac vein lesions, which are often occult, contribute to symptoms in patients with post-thrombotic disease, even when venous obstruction is more obvious elsewhere. Non-thrombotic compression in common or external iliac veins are present in about 60% of the asymptomatic general population, but may be found in more than 90% of symptomatic CVD patients. In many cases, treatment of these lesions helps alleviate symptoms.(4,5)
These compression stenoses can be identified in the common and external iliac veins of both the left and right legs with intravascular ultrasound (IVUS). (1)Since this initial report,multiple subsequent publications from these authors (3, 2007) have documented the safety and efficacy of stenting of CEIV and common femoral veins (CFV) stenosis due to compression or scar from prior acute DVT (“chronic DVT”) in CEAP 3-6 patients. In 2006, Neglen and Raju reported on 332 limbs where venography missed identifying an iliofemoral vein stenosis in 34% of studies while IVUS with venography showed greater than 90% diagnostic sensitivity. (3)
Murphy and colleagues also demonstrated higher sensitivity of lower extremity IVUS versus venography in a series of 33 patients undergoing treatment for iliofemoral deep venous thrombosis. (7) They reported that IVUS identified underlying venous lesions requiring intervention approximately twice as frequently when compared to venography [venography detected them in 16/33 (48%) while IVUS detected them in 33/33 (100%) (p<0.01)].
IVUS-Venography Debate
A significant stenosis on venogram is defined as a >50% diameter reduction. With IVUS, a significant stenosis is defined as a > 50% cross sectional area reduction. (CSAR). However, significant disagreement persists over whether venography alone is adequate to evaluate CEAP 3-6 patients for stenosis and subsequent stenting or whether IVUS is an essential tool for this evaluation. Neglen and Raju have reported an extensive experience with (single plane) venography and IVUS, for identifying significant CEIV and CFV stenosis. In 2006 they reported on 332 limbs (3). They showed that venography was only 66% sensitive (i.e. 34% of venograms appeared “normal”), whereas IVUS had a diagnostic sensitivity of >90% for identifying iliac vein occlusive disease.
However, proponents of venography argue that multi-planar views are necessary for proper diagnostic sensitivity. Proponents of IVUS, on the other hand, argue that not only does multi-planar venography miss a significant number of clinically meaningful iliofemoral vein stenoses but it is not as accurate for proper vein stent sizing. Intravascular ultrasound provides identification of obstructive or compressive lesions in the caudal inferior vena cava (IVC), iliac, and common femoral veins, and is very effective for guiding proper stent sizing and placement for endovascular correction of venous outflow obstruction.(5,8)
The VIDIO Trial
The VIDIO (Venography versus Intravascular Ultrasound for Diagnosing Iliofemoral vein Occlusive Disease) study is a prospective, single-arm, multi-center, study designed to compare multi-planar venography to intravascular ultrasound for diagnosing 1) common or external iliac (C/EIV) and common femoral vein stenosis; and 2) the extent, and morphology ( i.e. stenosis vs scar) of the occlusive disease. The patients involved must have CEAP 4-6 (clinical) disease and consent to the trial. Secondary endpoints include clinical (CEAP and venous clinical severity score (VCSS))and QOL (CIVIQ-14 and SF-36v2 questionnaires) improvement after intervention.
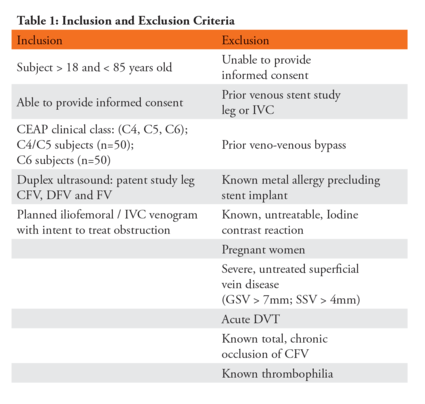
Venous ulcers were monitored and measured in CEAP 6 patients. Patients were evaluated for chronic venous obstructive disease due either to compression or scar from prior deep vein thrombosis (i.e. chronic DVT). Patients with complete occlusion of the iliac or common femoral vein or patients with acute DVT, were excluded. (Table 1)
The study is IRB approved and is being conducted at 13 sites in the US, Poland, United Kingdom and Italy. Enrollment was initiated in July, 2014 and completed in July, 2015. Clinical follow-up will be completed at the end of December, 2015.
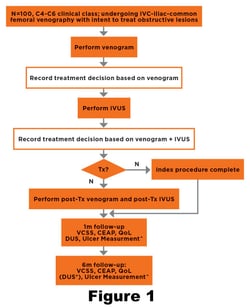
Consented patients underwent standardized, multiplanar venography (antero-posterior, 300 RAO and 300 LAO) of the C/EIV and CFV of the index limb (Lesser Femoral Trochanter to Inferior Vena Cava) to identify stenosis or obstruction. Based on these images, the investigator determined if there was a flow-limiting lesion requiring intervention with a PTA and/or stent. If yes, the type of intervention, balloon and stent to be used was to be stated.
The patient then underwent IVUS interrogation of the same C/EIV and CFV segments. Following IVUS, the investigator was asked again, if there was a flow-limiting lesion requiring intervention with a PTA and/or stent. If yes, the type of intervention, balloon and stent to be used was to be stated. Differences in identified intravenous pathology and intervention will be compared for the two imaging modalities.
Intervention was at the discretion of the investigator and was not defined by the protocol. Baseline, one and six month follow-up included venous duplex ultrasound, and the aforementioned clinical and QOL assessment tools. (Figure 1)
The VIDIO Objective
The goal of this study is to determine if significant additional diagnostic information is gained when the central deep veins of the lower extremities of patients with CEAP 4-6 disease are evaluated with both IVUS and multi-planar venography versus venography alone. The intent was to determine if clinically significant venous disease was missed when venography alone is used to evaluate these patients. Attention will be paid in the analysis to whether IVUS 1) identifies and characterizes additional, clinically meaningful deep vein pathology; and 2) whether IVUS alters the procedure performed compared to the plan following venography.
Half the patients (n=50) enrolled in this study were required to have active venous ulcers (CEAP 6). This design feature was created to try to gain insight from this pilot study into the challenges in performing a prospective study to evaluate the role of multi-planar venography, IVUS and central, lower extremity vein stenting for promoting healing inpatients suffering from CEAP 6 disease.
Though the study was not designed or powered to answer the impact of iliofemoral vein stenting for promoting
venous ulcer healing, we hope to gain some comparative data from baseline to six-month follow-up regarding the incidence of C/EIV and CFV occlusive disease in CEAP 6 patients as well as the healing response of these patients after venous stent placement. These insights will help to design further studies targeting improved treatment of the worst of CVI patients.
The results of VIDIO will be presented at the American Venous Forum in Orlando, Florida on February 24, 2016.
2. Semba, Dake. Et al. Iliofemoral deep venous thrombosis: aggressive therapy with catheter-directed thrombolysis . Radiology. 1994 May;191(2):487-94
3. Raju S and Neglen P. High prevalence of non-thrombotic iliac vein lesions in chronic venous disease: a permissive role in pathogenicity. J Vasc Surg 2006;44:136-44.
4. Bergan JJ, Schmid-Schonbein GW, Coleridge Smith PD, et al. Mechanisms of disease: chronic venous disease. N Engl J Med 2006;355:488-98.
5. Raju S and Neglen P. Chronic venous insufficiency and varicose veins. N Engl J Med 2009;360:2319-27.
6. Neglen, P, Hollis, KC, Olivier, J, Raju,S, J Vasc Surg 2007 46(5): 979–990.
7. Murphy EH, Broker HS, Johnson EJ, et al. Device and imaging-specific volumetric analysis of clot lysis after percutaneous mechanical thrombectomy for iliofemoral DVT. J Endovasc Ther 2010;17:423-33
8. Gloviczki P, Comerota AJ, Dalsing MC, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg 2011;53:2S-48S.