
In 2017, the American College of Phlebology (ACP) launched a collaborative quality improvement initiative with Johns Hopkins and the Robert Wood Johnson Foundation called the Improving Wisely Pilot Project in Vein Care.
As a community of physicians involved in caring for patients with venous disorders, members of the ACP have collectively shared concerns about overutilization of superficial vein procedures for the past several years. During the 2017 American College of Phlebology Annual Congress, there was an open forum discussion on ethical standards and overutilization.
At the heart of this is ACP members’ collective goal to provide the highest quality care to our patients in a safe, responsible, value-driven and cost-conscious manner. Many ACP members commented on overutilization of venous ablation codes, and I personally shared the success the Improving Wisely initiative had in my subspecialty of Dermatology.
The Power of Peer Comparison Feedback
Harnessing the power of comparison feedback and peer education to inspire changes in physician behaviors is at the core of the Improving Wisely Pilot Program. The program is based on the concept that transparency through peer comparison reduces unnecessary variations, which in turns leads to improved patient safety and quality of care while also reducing costs.
It works on the premise that all of us physicians are acting in the best interest of our patients and driven to provide quality care. Without national standards and benchmarking tools, many of us may operate our entire career without knowing how we perform next to our peers.
By providing confidential, individualized reports, Improving Wisely provides a collegial educational opportunity to help identify physicians who are unaware of their variations and bring their performance back into the norm.
Peer comparison feedback and Improving Wisely has a proven track record of success in modeling best practice behaviors in many industries. Many of you are familiar with monthly energy efficiency reports comparing your energy use against your neighbors.
Through the use of these peer comparison reports, the energy sector dramatically curtailed unnecessary electricity consumption. Similarly, handwashing compliance rate improved only after initiating individualized peer comparison feedback.
Currently, ongoing Improving Wisely initiatives include the American College of Cardiology, the American College of Gastroenterology and the American College of Mohs Surgery, of which I am also a member. While marked variations in the number of stages of Mohs surgery utilized per patient existed among physicians, the Mohs College identified that solo practitioners were at greatest risk of being outliers, which may be explained by limitation of collegial interaction, peer review, and feedback.
More importantly, a reassessment of the data several months after the original reports were sent to the providers demonstrated the use of confidential collegial feedback to physicians produced a change in individual practice patterns and reduced unwarranted variation. The educational benefit and feedback from members of other societies have been overwhelmingly positive.
The Improving Wisely Quality Collaborative Report
In the next few weeks, those physicians who performed more than 10 ablations in the past year on Medicare beneficiaries will receive a confidential individualized report by US mail from ACP’s Improving Wisely Quality Collaborative.
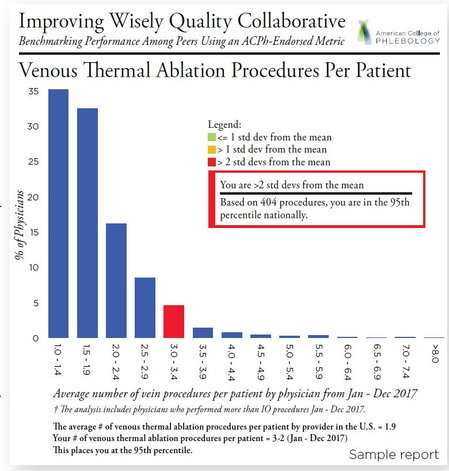
Using publicly available published payment data from the Medicare Provider Utilization and Payment Data from the Centers for Medicare and Medicaid Services, Improving Wisely prepared a provider-specific performance report showing each physician’s average number of vein ablation procedures performed per patient, and benchmarked this against national averages.
The national average proved to be 1.9 ablations per patient, with a median of 1.7. Of 2,462 physicians billing for venous ablation procedures, there were 106 physicians who were greater than two standard deviations above the average (i.e. 3.4).
The ACP hopes the Improving Wisely program will inform and educate vein care specialists as to how their practice patterns compare to their peer group and allow them to individually determine if improvements can be made in their personal practice.
Understand that the vast majority of physicians fall within two standard deviations of the mean. For those outside this range, there may be completely legitimate explanations based upon referral patterns, patient populations, numbers included in the database, and the like. The CMS claims data does not allow for risk stratifications and does not include younger private insured patients. It is hoped, however, that some will find an opportunity to identify patterns of practice that with modification could improve quality and value.
Mentorship and Support
Programs like Improving Wisely in vein care can demonstrate to all health care stakeholders that ACP’s members are dedicated to providing the best possible vein care. As a compendium to this pilot project, the ACP is creating educational and mentoring resources for members to improve their practice patterns.
The ACP’s Physician Engagement Committee is a small multi-specialty team that will be available for mentorship and education to support quality improvements for members and non-members. On the ACP website, a project home page open to everyone will be active that will curate frequently asked questions, general project documents, national-level data, and project milestones on Improving Wisely. This will be at http://www.phlebology.org/member-resources/improving-wisely.
As our new residents begin their academic year, I am reminded by how much my practice pattern, and that of my fellow faculty members, was shaped by our mentors. In turn, our ingrained variations in care perpetuate and imprint to the next generation, shaping their decision making. When asked why a resident chose a specific plan or surgical approach for a patient, it’s not unusual to hear “it’s how I learned it from Dr. X.”
To be sure, variations in care are inevitable; sometimes there is a lack of data for consensus, many times there is no single superior choice. How I guide a patient’s choice in treatment is influenced by a myriad of factors – some of which are unrelated to the disease state itself, like family issues, insurance, and self-care. There are legitimate reasons for practice variations that should not be discounted.
Improving Wisely simply provides transparency. There is something powerful about seeing how we perform relative to others; peer comparison feedback brings awareness and guides our practices in line with our peers. It’s time to abandon the notion of “it’s the way we have always done it.” Let’s harness the power of peer comparison to improve quality, enhance patient safety, optimize the value of service, and minimize overutilization.
Improving Wisely at ACP 2018
 On Friday, November 9, at the ACP’s Annual Congress, the Physician Engagement Committee (PEC) will present an analysis on the overall national data. Dr. Martin Makary, chief of Islet Transplantation Surgery and a professor of Health Policy & Management at John Hopkins Bloomberg School of Public Health, and head of the Improving Wisely Initiative will provide background and commentary in his Plenary Session Address.
On Friday, November 9, at the ACP’s Annual Congress, the Physician Engagement Committee (PEC) will present an analysis on the overall national data. Dr. Martin Makary, chief of Islet Transplantation Surgery and a professor of Health Policy & Management at John Hopkins Bloomberg School of Public Health, and head of the Improving Wisely Initiative will provide background and commentary in his Plenary Session Address.
A brief confidential survey will also be distributed regarding member attitudes toward this effort, the results of which will show aggregated data only, compiled by the Johns Hopkins statistical team.
Rest assured that the ACP and Improving Wisely team are committed to confidentiality. In the context of sharing data in the spirit of peer-based collaboration and quality improvement, these results are not legally discoverable and have no implications for board certification, membership or credentialing. Only the Improving Wisely staff has access to individualized data.
All results will be supplied to the ACP administration and the PEC in a blinded manner. All PEC members have pledged confidentiality in signed agreements. The PEC considered many measures and there was consensus for the initial quality benchmark in our pilot project. Other metrics will follow, but only after thorough vetting.
In 2019, the ACP and Improving Wisely will send additional reports with the same metric to allow physicians to track changes in their performance for education and quality improvement purposes.


