Pulmonary embolization (PE) is estimated to kill over 200,000 patients per year in the United States.[1] The scope of this increasingly recognized epidemic is broad and complex. The patient population is as diverse as it is large and spans the entire spectrum of age and illness.
Pulmonary embolization (PE) is estimated to kill over 200,000 patients per year in the United States.[1] The scope of this increasingly recognized epidemic is broad and complex. The patient population is as diverse as it is large and spans the entire spectrum of age and illness.
Treatment has historically focused on anticoagulation and reversal of the underlying risk factors when possible. The concept of inferior vena caval interruption to prevent PE has been around since the late 19th century but came into routine use in the 1970s with the advent of the Greenfield filter. Since the 1990s, the use of temporary, or retrievable, inferior vena cava filters (IVCF) has become common in the treatment of patients with deep vein thrombosis (DVT) and PE.
In fact, more than 250,000 filters are placed annually in the United States alone—far exceeding the rates in Europe or other places in the industrialized world.[2] In 2012, for example, implantation rate in the United States was remarkably 25 times higher than Europe (224,700 versus 9,070).[3]
The majority of these implanted filters are retrievable, but most are left as permanent implants despite no longer having an indication for use. Estimates for the dismal retrieval rates in the U.S. are often reported to be less than 20%.[4] Many potential complications have been attributed to indwelling filters, including increased risk of subsequent DVT, potentially catastrophic caval thrombosis, filter migration or perforation, disintegration, and embolization. These complications have led to adverse patient outcomes and multiple single and class action lawsuits.
In August 2010, and again in 2014, the Food and Drug Administration (FDA) formally published advisories reminding physicians of their responsibility for the devices they implant, and that they should be removed when the acute risk of pulmonary embolization has elapsed.[5] As a cardiology and peripheral vascular-based group practice at a 1,065-bed tertiary care community hospital, we sought to analyze our own institutional practices and design a comprehensive program to improve IVCF retrieval rates.
The poor IVC retrieval problem
The reasons for poor IVCF retrieval rates at our institution, and likely most others, is varied and multifaceted. First, practice guidelines pertaining to IVCF placement are often nuanced and even subtly conflicting depending on which subspecialty recommendation is followed.
This may lead to confusion among treating physicians and requests for unindicated placement. In many hospitals, ordering an IVCF is handled identically to any other low-risk procedure such as a chest X-ray or paracentesis—all providers have ordering privileges and the implantation is performed with a deference to the ordering physician regarding appropriateness. Additionally, the complexities of today’s highly specialized healthcare model offers other challenges related to IVC placement and follow up.
Patient care is often fragmented, especially in the inpatient setting, leading to poor care coordination and care transition. Details related to IVCF placement and scheduled retrieval are easily lost amid other complex hospital events and discharge instructions. It is not too uncommon for patients to be discharged with complete unawareness of an IVCF implantation. This is especially true in trauma patients, a population with historically dismal retrieval rates.
Finally, there remains a false sense of assurance or security following IVCF placement, a sentiment that has long permeated the medical community. Many patients are counseled to simply leave their filters as permanent implants by physicians unfamiliar with long-term complication data.
The “don’t worry, they have a filter” mentality may lead to underutilization of DVT prophylaxis on inpatients and potentially reduces the appropriate use of anticoagulation when indicated. In fact, physicians may assume that the presence of an IVCF reflects a prior or even current contraindication to anticoagulation.
The solution: a comprehensive program
For us, simply keeping a log of IVCF implants didn’t seem adequate to address the complexity and scope of the problem related to low IVCF retrieval rates. Issues at every level of care warranted a complete overhaul and, as a result, we built a comprehensive program from the ground-up to help address the impediments to optimal care. This program includes mandating a formal vascular consultation, management of an active follow-up database, referring provider education, management of anticoagulation, prescheduled retrievals, dedicated IVCF retrieval clinic, and continued quality and safety analysis.
The Consult
For a procedure involving the implantation of a medical device, especially one with the possibility of becoming a permanent implant, we feel that a formal vascular consultation should be the bare minimum first step.
The indications for placement, difficulty with follow up, management of complications, and potential medicolegal implications of IVCFs are simply too great to allow ordering privileges for all health care providers. Our group is comprised of cardiologists, vascular medicine specialists, and vascular-specialized nurse practitioners who help assess all patients referred for IVCF placement.
The formal consultation allows an upfront review of the patient’s medical history, an unpressured meeting with the patient to review the procedure, obtainment of informed consent, and review of the expectation of IVCF retrieval once the indication for temporary filter placement, if applicable, has elapsed. It also serves as an opportunity for education of referring providers and allows for further collaboration in situations where placement indications may be borderline.
Medical Management
Our comprehensive approach to patients with DVT/PE in need of IVCFs extends beyond simply reviewing placement indications to include management of anticoagulation. In scenarios where filters are placed due to contraindications for anticoagulation, we establish follow up appointments to review the continued need for IVC filtration, often re-challenging patients with anticoagulation after their work up or treatment is complete.
If an IVCF was placed for perioperative indications in high risk groups, such as required interruption of anticoagulation during the treatment period for acute DVT/PE, we provide formal perioperative instructions for anticoagulation management. Our service also assists with identifying which anticoagulation strategy may be most appropriate for a given patient based on their clinical presentation, laboratory parameters, and even financial capabilities.
We find that working directly with pharmacists, social workers, Coumadin clinics, and primary care physicians allows for more seamless care transition and improved adherence to the prescribed treatment.
The Database/Follow up
Tracking device implants is straightforward but requires perpetual attention. At our institution, we originally utilized a simple spreadsheet but have since migrated to a more sophisticated, HIPAA-compliant, online database. We have designated a single point person who is charged with logging, following, and charting each implant through until retrieval. The time investment for the management of our database varies, but conservatively requires at least 15-20 minutes daily for our typical practice volume (~ 100-130 implants/year).
Once an implantation is made, the decision for retrieval is designated and the patient is then categorized immediately for scheduled retrieval (e.g. – need for interruption of anticoagulation for surgery), scheduled IVCF clinic follow-up to review need for continued IVCF, or designated as a permanent implant. An incredibly important first step is obtainment of accurate patient contact information. When patients do not show for scheduled follow up appointments or retrievals, they are contacted by the nurse for rescheduling.
If patients are unreachable after multiple telephone attempts, or repeatedly fail to show for appointments, they are sent a certified letter from our practice explaining to them that they have a retrievable IVCF that we have in good faith repeatedly attempted to remove. This letter has contact instructions for our practice and its delivery is documented in the patient’s electronic medical record.
For patients who have moved, often out-of-state, and are unwilling to travel back for retrieval, we offer to assist them in finding a local physician for retrieval and help expedite getting their medical records sent to the appropriate person.
Components of a Comprehensive IVCF Program
Formal vascular consultation
- Review appropriate indications
- Establish expectations for retrieval
- Informed consent
Medical therapy
- Direct communication with consulting and/or primary physician regarding anticoagulation including treatment duration,
- medication options
- Assist with perioperative recommendations, if appropriate
Filter placement
- Permanent, temporary, convertible
- Document implantation in electronic medical record and notify primary care physician of procedure, indication, and expected retrieval time frame if appropriate
Database management
- Capture demographics, indications, filter type, expected duration until retrieval
- HIPAA-compliant, cloud-based database
- Frequent review by RN or administrator
Follow up
- Scheduled ideally at time of insertion
- IVCF Clinic for continued monitoring and decision making
- Clear methodology for reaching no show patients (documentation of attempted phone calls, certified letter)
- Assistance with arranged retrievals for patients that have moved (out-of-state)
IVCF retrieval
- Expertise with complicated retrievals (long dwell times, different types, tilt/migration, penetration)
- Use of variety of snares, balloon, laser Atherectomy, forceps, etc.
Continued assessment
- Ongoing program refinements
- Review best practices and latest guidelines
- Monitor for safety, referring provides education
Results
Prior to 2013 our cardiology-based group was tracking IVCF implants individually by physician, often coordinated loosely by each physician’s personal nurse or case manager. Even with this imprecise structure, retrieval rates were in excess of 70% for all filters designated as planned temporary implants, thus demonstrating the singular benefit of an active tracking and follow up system.
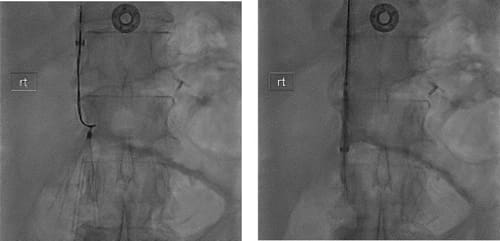
Starting in 2013, we combined all implanting physicians into a single managed database and prospectively tracked many important data elements including filter type, indication for placement, access site, dwell time, complications, presence of thrombus on retrieval, etc. Further refinements in late 2014 and early 2015 led to the comprehensive IVCF program described above. With this, we have further increased our success rates at retrievals.
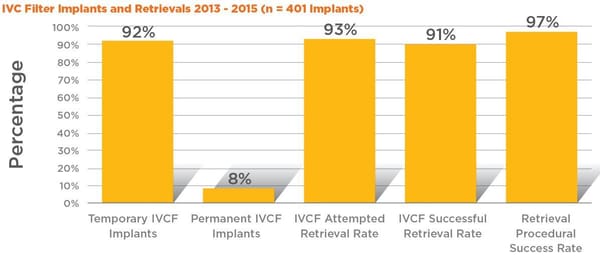
For example, from 2013-15, we implanted a total of 401 IVCFs. Of these, 369 (92%) were implanted as temporary filters with planned later retrieval; only 31 (8%) were designated permanent at implantation without plans for later retrieval.
We attempted retrieval of 93.2% of all filters deemed temporary at implant and were successful in removing 90.8%, a retrieval rate that far exceeds published rates for similar sized programs.
Procedural success at retrieval was 97.4%, a reflection of not only close follow up adherence but also an important marker of competency with the advanced retrieval techniques required to consistently maintain high retrieval rates.
“When used methodically, the implementation of a comprehensive IVCF program can dramatically improve not only retrieval rates, but even more importantly the appropriateness of implants and overall care of this diverse patient population.”
IVC Filter Implants and Retrievals 2013 - 2015 (n = 401 Implants)
Future Directions
Finally, our program seeks continued refinement and adaptation to evolving patient needs. The benefit of a well-organized database allows for reassessment, continued safety analysis, and real-time practice changes. For example, we have changed our preferred filter to reflect those with the best retrieval rates and lowest complications rates.
Additionally, we dramatically reduced our implantation of IVCFs for “softer” indications, such as bariatric surgery prophylaxis, when published literature and review of our own data demonstrated questionable benefit.
As we accrue more prospective data, we hope to gain further insights into areas such as risk modeling, which will potentially enable us to better predict those most likely to benefit from IVCF implantation. When used methodically, the implementation of a comprehensive IVCF program can dramatically improve not only retrieval rates, but even more importantly the appropriateness of implants and overall care of this diverse patient population.
Data continues to support the benefit of IVC filtration in highly selected patients, but only with careful steps to mitigate all possible risk can the full extent of this benefit be realized.
References:
- Silverstein MD, Heit JA, Mohr DN, Petterson TM, O’Fallon WM, Melton LJ. Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158(6):585-593.
- Angel LF, Tapson V, Galgon RE, Restrepo MI, Kaufman J. Systematic review of the use of retrievable inferior vena cava filters. J Vasc Interv Radiol. 2011;22(11):1522- 1530.e3. doi:10.1016/j.jvir.2011.08.024.
- Wang SL, Lloyd AJ. Clinical review: inferior vena cava filters in the age of patient-centered outcomes. Ann Med. 2013;45(7):474-481. doi:10.3109/07853890.2013. 832951.
- Sarosiek S, Crowther M, Sloan JM, et al. Indications, Complications, and Management of Inferior Vena Cava Filters. JAMA Intern Med. 2013;173(7):513. doi:10.1001/ jamainternmed.2013.343.
- FDA. Safety Communications - Removing Retrievable Inferior Vena Cava Filters: Initial Communication. http://www.fda.gov/MedicalDevices/Safety/ AlertsandNotices/ucm221676.htm. Published 2010. Accessed August 27, 2016.