 I am often asked a myriad of questions relating to the duplex examination for chronic venous insufficiency (CVI) or venous reflux. More and more physicians and technologists are entering the field of phlebology, from backgrounds and areas of medical specialty outside of traditional vascular surgery or otherwise outside the CVI construct. Over the past 10-15 years, I have come to observe that these non-traditional CVI physicians have some foundational knowledge gaps in key areas of CVI practice: duplex ultrasound procedures, protocols, and billing concepts.
I am often asked a myriad of questions relating to the duplex examination for chronic venous insufficiency (CVI) or venous reflux. More and more physicians and technologists are entering the field of phlebology, from backgrounds and areas of medical specialty outside of traditional vascular surgery or otherwise outside the CVI construct. Over the past 10-15 years, I have come to observe that these non-traditional CVI physicians have some foundational knowledge gaps in key areas of CVI practice: duplex ultrasound procedures, protocols, and billing concepts.
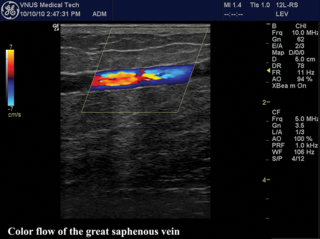
The first part of this article will dive into the subject of venous duplex ultrasound procedures and protocols. My discussion will focus on the two exam protocols endorsed by the Intersocietal Commission on Accreditation (IAC).[i] Interested readers can obtain copies of the protocols from the IAC website, which clearly describes two separate exam protocols.
In the second part, I will attempt to level set and better inform the readers of VEIN Magazine on the background of coding development and billing concepts, with input from my former colleague and longtime friend, Bill Schroedter. He is a seasoned expert in the field of vascular sonography, former Board Member and Vice President of the Society of Vascular Ultrasound (SVU) who also served as chair of the SVU Government Relations / Advocacy Committee.
This discussion will address a common complaint regarding the fact that venous reflux exams pay the same amount, using the same CPT code, as a venous duplex exam to rule out deep vein thrombosis (DVT).
Part 1
First, a few simple factual points regarding the IAC, vascular testing, and specifically its venous standards. The IAC is a nonprofit organization, with a list of sponsoring organizations which include:

The IAC’s document on vascular testing standards, just updated in August of 2015[i], can be found on the internet as mentioned just above. This is a 65-page document that goes through the various areas of vascular testing from Cerebrovascular (carotid) to Peripheral Arterial and Peripheral Venous testing, including the visceral testing, and content areas that include administrative, personnel, facility, safety and quality improvement to name a few in an exhaustive list of content areas. Of particular interest is the section on pages 41-47 on peripheral venous testing. These pages reveal a single place of information with overwhelming importance to anyone performing vein ablations or venous duplex examinations. There are two distinct protocols for venous duplex.
For quick reference, I like to refer to these as the “8/3 for DVT,” meaning 8 B-mode images and 3 Doppler images, and the “6/6 and 4 for Reflux” meaning 6 B-mode images, 6 Doppler images, and 4 Diameters as the minimum documentation requirements for each exam protocol. More documentation would be required to show the extent and severity of pathology in my opinion, and these protocols are based upon a written protocol that each facility should develop and follow on a daily basis. See below further information regarding these protocols and their documentation requirements per the IAC.
It should be noted that there are other recommendations for procedures involving vein mapping, venous stents, AV fistulas (or dialysis access grafts), that are not the subject of this article.
Additionally, the SVU has published performance guidelines[ii] for their members, last updated in 2014. These documents not only include protocols similar to those above, but also include some additional information like “exam time recommendations.” This is one of the other real “hot topics” of discussion for newbies. To level set the audience, see these recommendations which will set the foundation for the cost/reimbursement Q & A with Bill Schroeder below. The recommendation for a complete bilateral exam is 75 minutes for either protocol, and is broken down as noted below:
- Indirect time 15 min
Pre-exam activities: obtaining previous exam data; initiating exam worksheet and paperwork; equipment and exam room preparation; patient assessment and positioning; patient communication; post-exam activities: exam room cleanup; compiling, reviewing and processing exam data for preliminary and/or formal interpretation; and, patient charge and billing activities. - Direct exam time 45-60 min
Includes equipment optimization and the actual hands-on, examination process. Recommended time allotment is 40-60 minutes (for bilateral examination).

Part 2
 What follows below is a Q & A with some interesting information regarding the venous duplex CPT codes and their valuation with a well-known expert, Mr. William (Bill) Schroedter, BS, RVT, RPhS, FSVU. The venous duplex codes are 93970, which is for a complete bilateral exam, and 93971 for a limited exam (most performing a unilateral exam agree this to be the appropriate code).
What follows below is a Q & A with some interesting information regarding the venous duplex CPT codes and their valuation with a well-known expert, Mr. William (Bill) Schroedter, BS, RVT, RPhS, FSVU. The venous duplex codes are 93970, which is for a complete bilateral exam, and 93971 for a limited exam (most performing a unilateral exam agree this to be the appropriate code).
Joe Zygmunt: Bill, thanks so much for taking the time to participate in this process. The editors of VEIN Magazine greatly appreciate your time and expertise. For the first question, I’d like to ask if you could briefly describe the components that make up the valuation process for a CPT code for vascular studies, specifically the venous duplex exam? And perhaps how often these are re-evaluated?
William Schroedter: Let’s start with a little history. The American Medical Association (AMA) created, owns, and copyrighted the Current Procedural Terminology (CPT) code descriptions. The current codes (93970, 93971) for venous duplex ultrasound imaging have been in use since the 1980s and these are well established. The AMA participates in a number of specialized hybrid committees which are responsible for valuing the direct inputs for equipment, labor, and space, and making recommendations to the Center for Medicare/ Medicaid Services (CMS) about reimbursement policy.
“The first hurdle in addressing this issue would be to petition the AMA that a new CPT code for venous insufficiency studies is a distinct enough service to warrant a completely new procedure code.”
The following AMA Committees each have a role in this process.
- CPT Editorial Panel - Generates procedure descriptions based on input from the professional organizations for all procedures performed. Recommendations for any changes to code descriptions are forwarded to the AMA for review and approval and then the AMA recommends changes to CMS. If a CPT code is accepted by the Editorial Panel, it then needs to be valued.
- Practice Expense Advisory Committee (PEAC) - This committee reviews survey data to determine reliability and compliance with rules for evaluating data. The data must meet fairly rigorous and well defined standards to even be considered. If deemed acceptable, the PEAC makes recommendations to CMS for valuing the CPT code. However, the actual reimbursement is not set by the PEAC.
- Relative Value Scale Update Committee
(RUC) - Reviews PEAC data and evaluates physician work data, technical work data, equipment and space, and makes recommendations for valuation of CPT codes. The SVU Advocacy committee, typically working with the Society of Vascular Surgery (SVS) has been extremely active in this process over the past two decades. Data are collected from members and are then used in these descriptions. Most CPT codes are on a five-year review cycle. So to reiterate, it is not enough just to have the ACP or even multiple groups state that a venous insufficiency study takes 75” compared to a venous thrombosis study at 45”, this must be demonstrated by a well-defined survey process.
It is also important to understand that these committees determine only the “relative value” for a given procedure but it is actually Congress who determines what this Relative Value Unit (“RVU”) is worth and what we eventually get paid.
JZ: As I noted above, the SVU recommendations suggest that the time required to perform a DVT or Reflux exam is roughly the same. Is that the main reason why the reimbursement for the test using either protocol is equivalent?
WS: The SVU time recommendations really have little to do with code valuation and reimbursement. As I understand, these were developed in response to member requests for reasonable time guidelines. Members were and continue to be asked to perform more and more studies, which eventually raised concerns with regards to completeness and quality patient care, not to mention the health of the sonographer performing these arduous examinations. The time guidelines served to create a standard reference that sonographers could use to justify time spent on each exam.
JZ: Do you think there is any advantage in requesting a CPT code being developed (or two new codes) which would allow for the separate identification of a DVT vs Reflux exam? What do you see as the pros or cons of a two-code system?
WS: The first hurdle in addressing this issue would be to petition the AMA that a new CPT code for venous insufficiency studies is a distinct enough service to warrant a completely new procedure code. There are several mandatory criteria set forth by the CPT Editorial Panel which must be met prior to consideration of a new descriptor, a few of which are listed below:
- The proposed descriptor is unique, well-defined, and describes a procedure or service which is clearly identified and distinguished from existing procedures and services already in CPT.
- The proposed descriptor for the procedure or service is neither a fragmentation of an existing procedure or service nor currently reportable as a complete service by one or more existing codes (with the exclusion of unlisted codes). However, procedures and services frequently performed together may require new or revised codes.
- The structure and content of the proposed code descriptor accurately reflects the procedure or service as typically performed. If always or frequently performed with one or more other procedures or services, the descriptor structure and content will reflect the typical combination or complete procedure or service.
- The descriptor for the procedure or service is not proposed as a means to report extraordinary circumstances related to the performance of a procedure or service already described in the CPT code set.
A complete description of the process can be found here.
Given the same equipment, ultrasound room, personnel and ancillary services are used, this would likely be a heavy lift.
JZ: if a two-code system was developed, what impact do you think this could have on reimbursement for either exam type? As you may know, some new to venous reflux testing believe a reflux exam takes longer, and should pay more. What are your thoughts?
WS: As noted previously, if the CPT Editorial Panel agreed a venous insufficiency study was fundamentally different enough from a venous thrombosis study, there is a well-defined process by which a code is valued. This is carried out by the PEAC and RUC specialty committees which are comprised of members from a large number of physician specialty societies as well as member of the AMA, CMS and other stakeholders.
These meetings tend to be somewhat contentious given the fact that total reimbursement is generally a finite pie, and if one specialty gets an increase for a procedure they perform, the other specialty societies may see a decrease in reimbursement for procedures their members perform.
So there is an incentive to question and even contest the data being presented. One must also consider that the ultrasound room and sonographer time is only a piece of the expense valuation, any increase in reimbursement may not be worth the effort, especially given the CPT code for venous thrombosis could potentially run the risk of being devalued as the two-code system was considered.
JZ: One last question Bill, the Medicare LCDs have listed for many years, the idea that the venous duplex needs to be performed by a qualified person (RVT, RVS, or similar credential) for reimbursement by the governmental system. Do you have any idea if this is being broadly enforced, or at all? With Obamacare and perhaps other health care insurance changes, do you see enforcement of this policy gaining momentum?
“It is quite disheartening to think that the person who cuts your hair must be licensed to demonstrate minimal competence, but the person who determines if you have a life-threatening vascular condition can literally be anyone off the street. It is truly an indictment of our profession.”
WS: In particular, the SVU has been extremely active in this area. It took nearly two decades, but the SVU was able to convince Medicare Contractors that personnel credentialing was a necessary thing and would save money by ensuring a quality exam. As a result of these efforts, this requirement is now the standard for Medicare. Unfortunately, there has been absolutely NO enforcement of this fact as I understand it. I was told by more than one contractor director, they simply had no money to enforce this provision.
That said, if a provider submits a claim for a service not provided by a credentialed sonographer, it would in practice be a false claim. And here’s where it gets interesting—a provider who knowingly files a claim under such circumstances would run the risk of severe penalties (triple damages, $10,000 per claim, and potential exclusion from the Medicare program) but to my knowledge, a false claim suit has never been pursued against a provider for this reason. It is my belief, the only enforcement would come from sonographer licensure and in fact, two states now have licensure requirements for sonographers.
A national licensure requirement has been in front of Congress on multiple occasions over the past years but has failed to pass, opposed by several physician specialties and hospital groups. It is quite disheartening to think that the person who cuts your hair must be licensed to demonstrate minimal competence, but the person who determines if you have a life-threatening vascular condition can literally be anyone off the street. It is truly an indictment of our profession.
Thanks so much Bill for your comments, opinions and expertise on these interesting topics. Hopefully this will help those in the field better understand more of this complex landscape.
[i]Accessed 8/11/15; http://intersocietal.org/vascular/main/vascular_standards.htm
[ii]Accessed 8/11/15; http://www.svunet.org/svunet/membershipmain/membership
William (Bill) Schroedter is co-owner of an independent testing facility which exclusively performs vascular ultrasound and also co-director of Virtual Vein Center, an online learning resource. He has no pertinent financial disclosures. Bill has more than 35 years of experience in the field of ultrasound and served on the Society of Vascular Ultrasound (“SVU”) Board of Directors, was SVU Vice President and is past chair of the SVU Government Relations / Advocacy Committee. He has attended many of the AMA Specialty Committee meetings mentioned in this piece, as well as journeyed to CMS at Baltimore as well as Congress in DC as an advocate for quality vascular sonography. He was honored as a Fellow of SVU in 1998.
He continues to serve on numerous committees for SVU and the American College of Phlebology (“ACP”). Additionally, he teaches extensively throughout the country. He has authored dozens of publications, participated in numerous clinical trials, has been an invited speaker, nationally and internationally, and was honored as the International Keynote Speaker for the 2013 Australasian Sonographer Association Annual Conference in Sydney, Australia. In addition to his teaching and research activities, Bill still continues to perform diagnostic ultrasound nearly every day. Given the strenuous sonographer career, he advocates daily yoga practice for all sonographers and is also an avid conga player.
Joseph Zygmunt, RVT RPhS is well known to the readers of VEIN Magazine with his many previous contributions. He was also voted one of the “25 most influential” in our 2009 survey. Joe’s background as a skilled sonographer and owner/operator of three Vein Clinics give him unique insights into the challenges facing phlebology practice today.
Joe currently serves as Director of Ultrasound, Training and Portfolio advisor for Medtronic’s endoVenous business. Prior to his current role at Medtronic, Joe held a variety of roles within Covidien, where he focused on clinical education and served as a subject matter expert in venous diagnosis and disease states with the office of medical affairs and other cross functional responsibilities.
Disclaimer: The views set forth in this article represent the views and opinions of the individual authors, and do not represent the views of any of the authors’ current or former employers.


