by Carolyn T. Coffin MPH, RDMS, RDCS, RVT, BCOE
Many professions have documented work-related musculoskeletal disorders (WRMS D) for a number of years, and those industries have attempted to address injury risks. These injuries are defined as conditions that are caused by or aggravated by workplace activities, and they account for up to 60% of all workplace illnesses.1 Work-related musculoskeletal disorders (WRMS D) in sonography professionals have a reported incidence of 90%. These disorders are defined as conditions that are either caused by or aggravated by tasks performed in the workplace. These injuries have a financial and emotional impact on the worker and affect workplace productivity and quality patient care.
The causes for these injuries are multifactorial and, therefore, require a variety of solutions for mitigating injury risk. Sonographer work postures, work schedules, task rotation, administrative support and ergonomic workplace equipment all enter in the formula for reducing the incidence of these disorders. Injury among sonographers was first reported in 1985 when Craig identified “sonographer’s shoulder.”2 WRMSD’s were more extensively reported in surveys conducted in 1995 and 2008.3,4,5
Incidence of injury
According to an extensive survey in 1995, the incidence of musculoskeletal injury among North American sonographers was 84%.3 Manufacturers of ultrasound systems and exam tables have since incorporated ergonomic designs into many of their products, and some ultrasound education programs have added ergonomics to their curricula. Given this industry-wide awareness, it would seem that the occupational injury rate among sonographers would have been positively impacted.
However, a second survey in 2008 revealed the incidence of these injuries had increased to 90%.4 Possible explanations for this result may be due to an increased awareness among sonographers as to the reason for their fatigue and pain during the workday, a willingness to report their symptoms, and/or to increased workloads.
Causes for injury
The causes and contributory factors of these injuries in sonographers are numerous, but they can generally be grouped into three categories:
- Biomechanical/environmental factors that relate to the exam room size, the equipment in the room and the room’s set-up.
- Administrative factors that address scheduling of exams and sonographer rotation schedules, as well as unnecessary bedside exams.
- Worker practices – These are the postures sonographers use when scanning or working at a computer workstation, and are the one category of risk factors over which sonographers have the most control. Job satisfaction can also play a role in these injuries. Pressures and stress in the workplace have been identified as potentially affecting worker health.7
Other contributory factors are the aging workforce and increasing obesity rates.7 The impact of age is related to muscle force.8 By age 45, both males & females are approximately 10 years beyond their peak muscle strength since maximum muscle strength is reached in the 2nd and 3rd decades.8 Obese patients require the sonographers to exert more force during the ultrasound exam and may require an extended reach and/or excessive arm abduction to access both sides of the patient.
High-risk work activities
The work activities that can lead to WRMSD in sonography are forceful or awkward movements, duration of pressure, overuse, poor posture or improper positioning, excessive force and strain.9
The duration of pressure used during a vascular exam is related to the amount of time that the sonographers are actually scanning, or “transducer time,” and to the amount of transducer pressure being exerted while scanning.

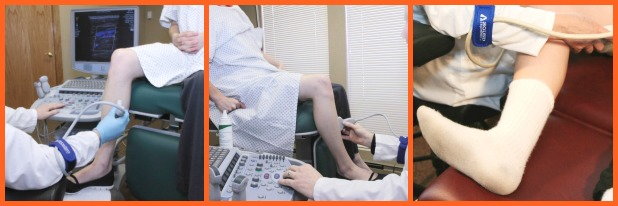
Poor posture and improper positioning of extremities (shown above) include:
- wrist flexion and extension
- neck twisting or extension
- trunk twisting and flexion and reaching
- arm abduction.
Static work postures reduce blood flow to the joints, which then increases the load on the muscles and decreases the time for fatigue to occur.
High-risk work postures
A common static work posture among sonographers is abduction of either the scanning arm or the non-scanning arm. An angle of abduction greater than 30 degrees puts the shoulder at risk for injury, especially if the arm is abducted for long periods of time.18, 20 Sonographers often scan with excessive arm abduction because they do not take the time to optimize their position with respect to the patient and the ultrasound system.
Overreaching beyond 30 cm for a prolonged period of time is another common injury-producing work posture.16 Clinical site work evaluations have demonstrated that the amount of reach for a sonographer to scan the left side of a patient’s abdomen or the left lower extremity can be as much as 63 cm (pictured below).
Forward reach to the ultrasound control panel varies depending on which controls are being accessed and the design of the control panel, but when sonographers rest their non-scanning arm on the ultrasound system at a distance in excess of 30 cm, the risk for injury increases.
Injury-producing work postures are especially prevalent when performing venous reflux exams. Typically, these are performed with the patient standing, either on the floor or on a step stool, which forces the sonographers to sit on the floor (pictured below). The resultant work postures are excessive reach, particularly with the non-scanning arm, excessive neck extension and trunk twist.
In addition to abduction and overreaching, performing exams with the scanning arm behind the shoulder, reaching across the front of the body to access the control panel and scanning with the arm unsupported can all put strain on the shoulder.

Holding the Tranducer: Pincher vs. Palmer Grip
Transducer designs can often force the use of a “pinch” grip rather than a whole-hand, or palmar grip. Since ultrasound manufacturers cannot produce a transducer for each individual user, sonographers must learn to hold the transducer in a more comfortable grip.
 A “pinch” grip uses the smallest muscles of the body and requires up to five times more muscle and tendon force than a palmar grip.21 Therefore, sonographers should try different ways of holding the transducer that uses more of the whole hand.
A “pinch” grip uses the smallest muscles of the body and requires up to five times more muscle and tendon force than a palmar grip.21 Therefore, sonographers should try different ways of holding the transducer that uses more of the whole hand.
Best practices for mitigating sonographer occupational injury
Preventative measures can range from simple work posture changes that conform to the department’s existing equipment to upgrading the department with state-of-the-art ultrasound systems, exam tables and chairs. However, all the best equipment is only as good as the willingness of the user to optimize the features of that equipment and to make work posture changes. Therefore, it is a combination of factors that has a positive impact on reducing injury risk hazards.
Sonographers should sit or stand so that they can move down the length of the exam table when necessary to prevent reaching back while scanning. They should also position themselves in front of the most frequently used keys on the ultrasound control panel to avoid reaching across their bodies. Strain on the shoulder can be reduced by using an arm support device while scanning.
Both arm abduction and overreaching can be reduced by lowering the exam table, and/or raising the chair by having the patient move close to the sonographer and by positioning the ultrasound system’s control panel close to the sonographer.
A qualitative study looked at the reduction in muscle firing when the scanning arm was supported. This was evaluated using surface electromyography (SEMG) that provided audible feedback. Muscle firing, as determined by the beeping of the SEMG unit, was significantly reduced when using the arm support device.23
When scanning the patient’s neck for carotid artery exams, the sonographer should scan from the head of the table, facing the patient’s feet (pictured below). They should also try having the patient sit for these exams and then stand behind him/her. This allows the sonographer to be close to the patient and to position the ultrasound system close. It also gives the sonographer the opportunity to rest his or her forearm on the patient’s shoulder.

To reduce abduction and reach when performing bilateral or left lower extremity venous exams, the sonographer should have the patient turn around on the exam table and lay with his/her left leg closest to the sonographer (pictured above). Although this may not be possible with patients who have limited mobility, the goal is to make work posture changes as often as possible so that awkward and/or static work postures are only used when there is no alternative.
Another option for lower extremity exams is to have the patient sit with his/her legs dangling over the edge of the exam table close to the sonographer (shown below). In addition, sonographers should have cooperative patients perform self-augmentation during lower extremity venous exams by flexing his/her foot toward the knee. This eliminates neck and trunk twist when reaching to compress the patient’s calf.
Venous reflux studies can be more comfortably performed by the sonographer with the patient lying on an exam table. This achieves an angle of reverse Trendelenberg of at least 40 degrees. The sonographer should then position himself/herself at the foot of the exam table, sitting or standing at a height that reduces arm abduction and reach (shown below). In addition, an ultrasound system with a height-adjustable control panel that can achieve a minimum height of 24” reduces the need to reach up to access the controls and reduces neck extension when viewing the monitor (shown below).

Not all exams can be performed every time with optimal work postures. However, the more often sonographers can use neutral work postures throughout their work day, the lower their risk for WRMSD.
Environmental changes
Although changes in work practices are pivotal in addressing injury risk, administrative support and biochemical/environmental changes are also important components. Department managers should establish a work environment in which sonographers feel comfortable reporting injuries and addressing risk hazards. Managers should be receptive to changing work schedules so that sonographers rotate through a variety of exams and are not repeatedly exposed to high-risk exams without some muscle recovery time. Patient exams should be scheduled with enough time for sonographers to optimize the exam room setup for each exam.
The desire to provide patients with a positive experience should be balanced with the need to provide quality, diagnostic exams while still maintaining a level of worker comfort. This is of particular concern with in-patients and bedside exams. In an effort to prevent patients from having to travel to the ultrasound department or to accommodate the nurses’ schedules, many ultrasound exams are needlessly performed at the bedside. These can be among the most injury-producing exams for sonographers since it is not easy to optimize equipment placement in the patient’s room or to move the patient into an accessible position. This results in sonographers having to bend and/or twist to reach the patient throughout the exam. Although these exams should be reserved only for those patients whose health would be compromised if they were to be transported to the ultrasound department, the growing trend of providing all patient services at the bedside has created the need to find innovative ways for sonographers to work in more neutral and comfortable positions during these exams.
Correct scanning postures are more easily and more consistently achieved when the workstation equipment has multiple ergonomic features. All workstation equipment must be adjustable in order to address the physical dimensions and work style of each sonographer in the department. Monitor position should be easy to adjust and the control panel should have a wide range of height adjustability. The system should be easily moveable so that it can be positioned close to the exam table. (below)

The exam table should be height-adjustable by electric controls. It should go low enough to accommodate wheelchair transfers and to perform lower extremity exams, and high enough to allow sonographers of various heights to stand during exams. Other exam-specific features can be added that enhance the ergonomics, such as a detachable arm board for upper extremity exams. And, finally, the exam room chair should have an adequate height range to accommodate the position of the table throughout each exam. All exam room equipment should be quick and easy to adjust; otherwise, sonographers will not take the time to optimize the features of the equipment.
Conclusion
Work-related musculoskeletal injuries among sonographers can impact the quality of patient care, can have a financial impact on both the ultrasound department and the individual worker, and can negatively affect the morale of the workplace. The multiple causes of these injuries require multiple approaches to their prevention. At the center of any injury prevention program, however, is the participation of the worker. Sonographers must recognize injury risk hazards, utilize the ergonomic features of their workstation equipment and be willing to make changes in their work postures. The administrative environment of the sonography workplace must support these attempt to change and to report injuries. Without this synergy, it is difficult to effectively reduce the incidence of workplace injuries.
References
2. Craig M. Sonography: An Occupational Health Hazard? JDMS. May/June 1985; 1: 121-125
3. Pike, I, Russo A, Berkowitx J, Baker J, Lessoway V. The prevalence of musculoskeletal disorders among diagnostic medical sonsgraphers; JDMS; Sept.-Oct. 199713(5): 219-27
6. Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta analysis. Occup Environ Med. 2005;62: 105-1128. Lowe GS. High-quality healthcare workplaces: A vision and action plan. Hospital Quarterly; Summer 2002: 49-52
7. http://www.cdc.gov/obesity/data/adult.html
11. Russo A, Murphy C, Lessoway V, Berkowitz J. The prevalence of musculoskeletal symptoms among British Columbia sonographers. Appl Ergon; Sep 2002; 33(5):385-393
12. Roll SC, Evans KD, Hutmire CD, Baker JP. An analysis of occupational factors related to shoulder discomfort in diagnostic medical sonographers and vascular technologists. Work; 2012; 42(3):355-365
13. Rempel DM, Harrison RJ. Barnhard S/ Workrelated cumulative trauma disorders of the upper
extremity. JAMA; Feb. 1992; 267(6): 838-842.
15. DeKron ACTFM, Kester ADM, Knipschild PG. Risk factors for carpal tunnel syndrome. Am J of Epidemiology; (1990) 132(6):1102-1110.
16. Kroemer KHE, Grandjean E. Fitting the Task to the Human, 5th edition, chapter 1.
17. Village, et al. Ergonomic analysis of postural and muscular loads to diagnostic sonographers. International Journal of Industrial Ergonomics; 2007; 37(9-10):781.
18. Vedsted P, Blangsted AK, Soggard K, Orizio C , Sjogaard G. Muscle tissue oxygenation, pressure, electrical and
mechanical responses during dynamic and static voluntary contractions. Eur J Appl Physiol (2006) 96:165-177.
19. Nussbaum MA . Static and dynamic myoelectric measures of shoulder muscle fatigue during intermittent dynamic exertions of the low to moderate intensity. Eur J Appl Physiol (2001) 85: 299-309
20. Pennett L, Fine LJ, Keyserling WM, Herrin GD, Chaffin DB. Shoulder disorders and postural stress in automobile assembly work. Scand J Work Environ Health (August 2000) 25(4): 283-291.
21. Hill JJ 3rd, Slade MD, Russi M. Anthropometric measurements, job characteristics and prevalence of musculoskeletal symptoms in female medical sonographers. Work (2009) 33:181-9.
23. Murphey S, Milkowski A. Surface EMG evaluation of sonographer scanning postures. JDMS (2006) 22(5); 298-205.


