
MEDICINE IS A discipline built on a spirit of collaboration that continually advances because it learns from itself. The mantra, “See one, do one, teach one,” describes the transfer of knowledge inherent to medical training, and it helps explain why physicians favor education models predicated on peer-to-peer interactions.
On a basic level, collaboration requires access, meaning individuals being in the same place at the same time, while sharing knowledge. When new technologies and surgical techniques become available, proctoring and industry support of early cases facilitates correct usage. As questions arise over time, the ability to consult with expert colleagues and industry representatives is critical for maintaining ongoing collaboration.
Facilitating collaboration has always been challenging. Sustaining access requires significant expenditure, coordinating schedules, and managing complex logistical realities. The COVID pandemic has amplified these issues while also introducing new concerns that interfere with peer-to-peer and peer-with-industry collaboration. Travel restrictions, social distancing, and requirements for isolation speak to just a few of the current practical limitations. At the same time, new economic realities are constraining budgets and putting pressure on industry and medical providers to do more with less. Perhaps most importantly, ensuring patient safety means reducing the number of people entering hospitals, procedure rooms, and ambulatory surgery centers (ASCs), which further reduces the ability for physical access to collaborate.
Adapting to the demands of the “new normal” in medicine will require us to rethink how things are done on a daily basis to assure consistent delivery of high-quality care, including a conversation about how medicine continues to foster the collaboration that allows members of the health-care community to grow their expertise for the betterment of patient care.
The Many Forms of Collaboration
Innovation is the lifeblood of new ideas in medicine. The vein market is one of the most exciting to track. New procedures and technologies—whether for vein ablations, stenting procedures, or other indications—are introduced at a rapid pace and greatly facilitate collaborative interactions during integration and through regular use in practice.
For example, both device introduction and integration are highly reliant on physician-with-industry interactions. Industry plays a role in helping physicians manage learning curves for new technology, training on the steps involved in using a new or novel device, appreciating the nuances in technique, and learning to troubleshoot. Such collaboration has historically required an industry representative to visit a clinic, which can be costly as well as logistically challenging for both the industry representative as well as the treating physician and clinic.
The amount of effort required for all parties can be seriously undermined if the planned case is rescheduled or canceled. Other forms of collab-oration, particularly direct peer-to-peer interaction, are profoundly important for the dissemination of knowledge and expertise. In-person conferences, medical meetings, and symposia are clear examples. Less obvious is the clinical trial investigator who goes out into the field to share experiences with colleagues. Or the technique innovator who proctors a colleague’s procedure or surgery. Or the reverse, where a physician in one part of the country (or world) wishes to travel to a site in another part of the country (or on another continent) for a live procedural learning experience with a renowned expert.
Finding Solutions Through Technology
The emergence of the COVID pandemic has challenged and reshaped medical practices in numerous ways. Cost realities have impacted many organizations; we are facing an unprecedented need to fund innovations to keep employees and patients safe while continuing the advancement of health care. This means we need to look for ways to do more with less and to be more efficient whenever possible.
At the end of the day, this crisis has shown us that medicine is malleable, and health-care providers are willing to adapt to meet their duties to provide high-quality care. It has also shown us we are capable of a level of comfort with remote and digital communication that previously may not have been considered realistic. The COVID scenario, in essence, has created a call to action for technological innovation in health care.
Procedural Telemedicine & Avail
For me, as a medical device executive, innovation is about solving a problem. In my previous role as founder and CEO of Shockwave Medical, a company focused on developing and commercializing products intended to transform the way calcified cardiovascular disease is treated, I witnessed firsthand the struggles medical technology companies face in getting their products in front of physicians and teach-ing them how the devices work, despite the importance of innovation to advancing care. I saw medical device representatives spending more time traveling or waiting for procedures to start than time actually working with physician customers to support product rollouts or training. I also observed medical providers who wanted to collaborate with or learn from peers face equally daunting logistical challenges as well as tradeoff decisions about whether to miss a day in their own practice or miss a coveted education opportunity.
 I knew there had to be a better, more efficient way for the medical industry to collaborate to grow new technologies. In 2017, I launched Avail, a novel procedural telemedicine solution. I sought to enable seamless collaboration between medical experts, even when they’re not able to be in the same room. With Avail, I envisioned a scenario where device companies roll out technologies quicker and with less cost, and physicians can improve their skills by instantly tapping into the top experts in their field without the complex logistics of travel.
I knew there had to be a better, more efficient way for the medical industry to collaborate to grow new technologies. In 2017, I launched Avail, a novel procedural telemedicine solution. I sought to enable seamless collaboration between medical experts, even when they’re not able to be in the same room. With Avail, I envisioned a scenario where device companies roll out technologies quicker and with less cost, and physicians can improve their skills by instantly tapping into the top experts in their field without the complex logistics of travel.
Fast forward two and a half years, and we are more than six months into a truly unprecedented time. All the burdens of in-person collaboration that caused me to launch Avail are not only magnified but, in many cases, in-person collaboration is no longer possible. Rather than having to rush to build a new system for the new normal, Avail was already methodically designed and built for the procedure room.
The fact that Avail specifically designed its technology for use in procedural telemedicine has provided us with a leg up over other platforms (those that were designed for patient telemedicine, for example) that are being reversed engineered in an effort to provide this same functionality. As a result, users have told us our purpose-built platform provides greater functionality and easier integration than other systems they’ve tested.
Our service structure was also thoughtfully predicated on removing barriers to implementation. For example, Avail is offered with a subscription-based fee model rather than capital costs, and our field operations and implementation team spends time in the clinical facility to ensure integration.
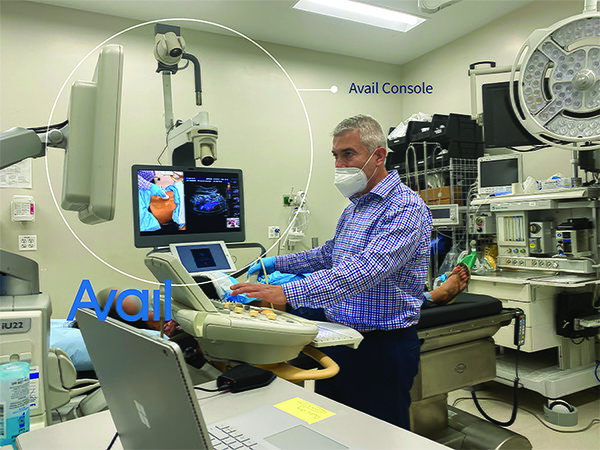
Avail designed a solution for problems that already existed, and now, when those problems are exacerbated by the pandemic, our solution gives users confidence from day one that their procedural telemedicine platform will be easy to use, not interrupt regular duties and ideally, expand possibilities for collaboration. Avail provides a fully interactive, virtual, collaborative experience for remote users and treating physicians as well as tools to manage schedules and availability for both parties. The system consists of a mobile console that sits in the operating or procedure room, two high-definition pan-tilt-zoom cameras, plug-ins for external imaging, and a large display monitor controlled by the remote user(s). On the other side, a physician, medical device representative, or other health-care professional uses our remote app on a touchpad device or laptop computer to see the camera and imaging views streamed from the console in real-time.
Through the app, users can control camera positioning and zoom up to thirty percent to get up-close views not otherwise possible with the naked eye, annotate directly on-screen, split the screens to view inputs side by side, and freeze frames. These capabilities provide a content-rich environment for medical advisors and can be more powerful than trying to see around medical equipment and other people when physically present in the room.
Both parties can communicate audibly with each other through an advanced audio system designed for the procedure room. The entirely self-contained and mobile platform has a small footprint, requires no new construction, can be moved and paired to different rooms, and can integrate with imaging sources regardless of brand.

Avail Remote App, accessible from iPad or laptops, allows remote users to control camera movement and zoom, switch between camera and imaging views, annotate, and communicate with the treating physician.
Very recently, Avail announced the launch of the new Avail Portal, a tool I’m really excited about. It connects the network of health-care and industry experts for seamless collaboration. The secure portal, accessible via Avail.io, allows system users to easily manage schedules, update availability in real-time, and connect with each other at the click of a button.
The Future of Remote Access Procedure Collaboration and Medical Education
The COVID pandemic has forced a reckoning on health care, and its effects will have a lasting legacy on patient interactions and collaboration in its various forms. As clinicians everywhere have become more comfortable with telemedicine for patient interactions and more acquainted with using digital communication platforms, there is an opportunity to use what we have learned to facilitate a new era of procedural telemedicine.
Avail’s collaboration with the organizers of the recent Venous Symposium this past July highlights many of the advantages of our platform in just one application. In previous years, streaming a live case to an educational seminar meant sending a camera crew to a remote procedure room, entailing significant cost and logistics, and potentially affecting patient comfort with so many people in the room.
Dr. Nicos Labropoulos at the recent virtual Venous Symposium using the Avail System to stream live video and ultrasound imaging to the remote symposium audience.
Now add the fact that COVID limits people being in the room as well as the reality that major medical conferences and meetings are being held online. The demand for high-quality education is still present, and our system provided a less-disruptive means to do just that, even under these trying conditions. During the meeting, live cases were streamed directly to the symposium’s virtual attendees.
While so much has changed because of COVID, one thing that will remain important for the advancement of medical care is the close collaboration between physicians and with industry. Avail fundamentally solves the problem of access by removing barriers associated with in-person collaboration. Even before a global pandemic entered into our consciousness, cost and logistical realities suggested a need for a more effective and efficient system for providing training, education, and technical support across all sectors of health care. Our recent work with the organizers of the Venous Symposium provides one example of how our technology can be applied in the realm of medical education.
As Avail looks to the future, we see numerous ways in which our technology provides the means to work smarter instead of harder to accomplish seamless collaboration between physicians and with industry.


