By Dr. Thomas Wright
Lipedema is characterized by painful and swollen fat which accumulates disproportionately in the subcutaneous tissue. New studies have shown that all stages of lipedema show increased swelling in the lower extremities as measured by Bioimpedence. In a study published this year in the Journal of Lymphatic Research and Biology, Crescenzi, Donahue, and Herbst showed that compared to controls all stages of lipedema have increased extracellular water or swelling. (R. Crescenzi, 2019) Further, the study showed that the edema or extracellular water increased with each stage of lipedema. We know that extremity edema or lymphedema is associated with multiple inflammatory processes that are responsible for pain, tenderness, and progressive fibrosis of the affected areas. All the Standard of Care [Dutch (Damstra, 2017), German, and British (Coppel, 2017)] Guidelines for the management of lipedema recommend the use of compression for patients with lipedema [Stage 2,3]. All of the care guidelines recommend a multidisciplinary approach to treatment involving lymphedema therapists teaching patients manual lymphatic drainage, proper fitting compression garments, and instruction on the proper application of the compression garments. Therefore, we conclude that compression is usually needed in stage 1 lipedema and always needed in stage 2 and 3 lipedema.
What is the Goal of Compression Therapy in Lipedema?
The goal of compression therapy in lipedema is:
- reduce discomfort, aching, and limb heaviness as well as supporting the health of the tissue.
- help to streamline uneven or distorted limb shape and improve movement.
- help to reduce edema by reducing the interstitial fluid formation and encourage venous and lymphatic return in lipedema. (Hardy, 2016)
All three goals are critical for the management of lipedema. Compression is the cornerstone on which all other treatments for lipedema are built upon as it is the only treatment that has been shown to benefit every patient with lipedema. Studies have shown medical-grade graduated compression is the most universally applied effective treatment for reliving limb heaviness, tenderness, and leg cramping and it should be the first line of treatment for lipedema as it is an extremely low risk and relatively low cost and readily available treatment. Compression with or without other lymphatic stimulating treatment is an effective first line of therapy for managing lobules, wrist, and ankle cuffs that occur with lipedema.
How Graduated Compression Likely Deters Progression of Lipedema
While the exact pathogenesis or pathogenic mechanism by which lipedema develops is not known, all current understanding points to the lymphatic system playing a role in the development and progression of lipedema and its symptoms. Medical grade graduated compression has not only been shown to treat symptoms of lipedema and correct lobules and ankle and wrist cuffs caused by lipedema, but also compression has been shown to optimize lymphatic flow and encourage draining of inflammatory interstitial fluid. The excess interstitial fluid and its inflammatory proteins and signaling agents seen with lipedema is responsible for nodular fibrosis, lobular fibrosis and progressive dermal fibrosis that occurs with lipedema. The progression of the fibrotic processes is highly linked to disability from lipedema.
Individual Recommendations for Compression with lipedema?
The optimal strength of compression depends on the individual patient and her stage of disease. Of course, there are a few individuals with early Stage 1 lipedema who may not have any detectable interstitial edema or lymphedema who may not need medical grade compression. Even this can be a bit tricky because most individuals with characteristic disproportionate fat consistent with early stage lipedema are not symptomatic, so may not technically meet the diagnostic criteria for lipedema. These individuals still would likely benefit from compression garments. Perhaps; however, individuals with early symptomatic lipedema do not need medical grade graduated compression and would suffice with compression garments that are not graduated or medical grade.
Compression garments that are not graduated and were originally designed for post-operative recovery have a uniform compression strength of generally 12-20 mmHg. The non-graduated post-surgical garments do not aid significantly in the flow of lymph. Compression garments sold by manufacturers like Bioflect, Marena, and Veronique and Copper Fit are very popular, but they are not recommended for any individual with symptomatic lipedema as they are not graduated and are not medical grade. Almost all individuals with lipedema have excess interstitial fluid or lymphedema and therefore should be treated with medical grade graduated compression applied to the areas of the body that are affected. Quality Medical Grade Graduated Compression are made by brands such a Jobst, Medi, and Sigvaris.
What Is Graduated Compression?
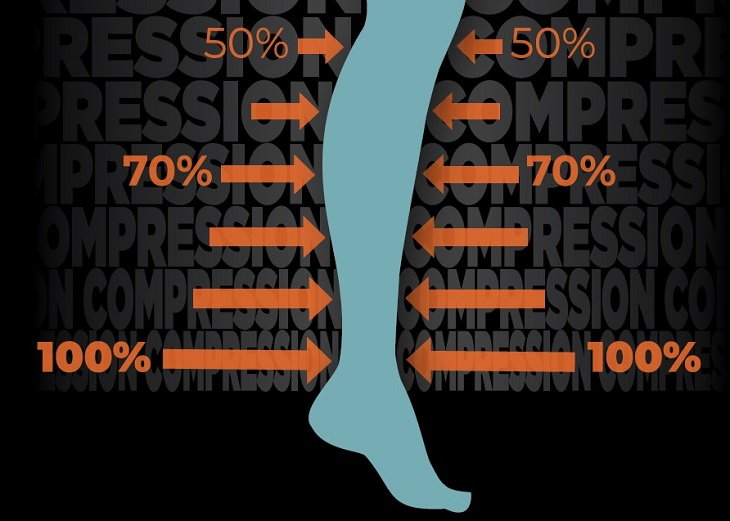
Graduated compression is based on the principle that fluid flows from higher pressure to lower pressure. So to encourage the interstitial fluid or edema that builds up in lipedema to exit or flow out of the affected limbs the compression of the garments must be greater in the end, distal portion, of the limb and gradually lower pressure until the limb joins the body. The principle of graduation is followed in the graduate garment such that maximal pressure or 100% compression strength is applied to the distal end such as an ankle or wrist, then 70% of the compression strength is applied to the calf or forearm. This gradual decreased pressure continues such that the knee or elbow has the approximate compression of the distal end and the thigh or upper arm usually has 30-40% of the maximum compression pressure. Almost all graduated compression is medical grade, which studies have shown the pressure strength measured in millimeters[mm] of Mercury [Hg] to be high enough to help moderate of higher edema.
What Pressure is Considered Medical Grade and Recommended for Lipedema?
Medical grade compression strength varies by the affected limb and the severity of the edema or fluid accumulation. An arm requires less compression to aid lymph flow because it is both smaller than a thigh and closer to the heart so under less gravitational pressure difference. In general, 18 -20 mmHg [Mercury] is considered medical-grade compression for the arm, and 30 - 40 mmHg strength at the ankle is considered a medical-grade compression strength for the leg. These recommendations are based on studies primarily of primary lymphedema as this is the strength required to cause a significant improvement in lymphatic flow. (Mosti, 2019) The studies of compression garments show those [e.g. 30-40 mmHg ankle and 18-20 mmHg wrist] pressures give both optimal venous blood flow and lymphatic fluid clearance from the affected limbs. There need to be more studies of compression effectiveness in lipedema. Sometimes compromises are made, and lower 20-30 mmHg compression is used for individuals who have very mild edema or who are just starting to use compression garments or because of extreme sensitivity to the pressure of the compression.
Ideally, the lower 20 -30 graduated compression is used as a stepping-stone until the heavier compression can be tolerated because the evidence for this lower strength of graduated compression controlling interstitial fluid is much weaker and not as trustworthy. While it is yet to be proven that proper compression can reduce the progression of the lipedema at this time, the recommended graduated 30-40mmHg pressures at the ankle have been shown to be effective at minimizing edema, reducing symptoms and halting the progression of the disease in closely related lipedema, veno-lymphedema, and other diseases that are known to cause secondary lymphedema and therefore 30-40 mmHg strength at the ankle must be the goal of compression therapy.
Compression Physiology and How Compression Works in Lipedema
When considering the use of compression therapy in the management of lipedema, the basic principles should be understood. The law of Laplace is a mathematical formula that defines the relationship between pressure P, tension T, radius R, and garment layers N.
The law of Laplace
- P relative to N T/R
- P = pressure
- N = number of layers T = tension applied = radius of limb
Special Needs and Flexibility with Compression in Lipedema
Compression garments are hard to fit for women with Lipedema. By definition, the fat accumulates out of normal proportion on the bodies of individuals with lipedema, which leads to unique body shapes. Often hips, thighs, and calves will be much larger on individuals compared to the rest of their bodies. These size differences necessitate flexibility with compression garments and layering of multiple compression garments. One of the most successful combinations for coverage of the legs is to get knee-high socks with 30-40 mm Hg compression strength at the ankles and layer it with Capri length compression pants that overlap at the top of the calf. This combination gives comprehensive coverage for the entire lower extremity without gaps. Another combination that is very effective for patients with lipedema is thigh-high compression stocking layered under compression shorts that go to the top of the knees. The compression shorts help hold the thigh stockings in place. Not only does the layering of the garments help hold the garments in place it also allows for the garments to be different sizes.
References:
- Best Practice Guidelines: The Management of Lipoedema. Wounds, UK, 13(1), Vol 13, No 1. Retrieved from
https://www.lipoedema.co.uk/wp-content/uploads/2017/05/WUK_Lipoedema-BPS_Web.pdf
https://www.ncbi.nlm.nih.gov › books › NBK545818 - Damstra, R. (2017). The Dutch Lymphedema Guidelines Based on the International Classification of Functioning, Disability, and Health and the Chronic Care Model. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 5(5), Vol. 5, Number 5. doi:
www.ncbi.nlm.nih.gov/pubmed/28818234.
https://www.ncbi.nlm.nih.gov › pubmed - Hardy, D. (2016). Best Practice Guidelines for the Management of Lipoedema. British Journal of Chronic Edema, https://www.ncbi.nlm.nih.gov/pubmed/28961048.
https://www.ncbi.nlm.nih.gov/pubmed/20559170 - Mosti, G. (2019). Compression Therapy in Lymphedema: Between past and recent scientific data. Phlebology, 34(8), 518-522. https://lymphoedemaeducation.com.au/resources/compression-therapy-in-lymphedema-between-past-and-recent-scientific-data/
- R. Crescenzi, P. D. (2019). Lipedema and Dercum's Disease: A New Application of Bioimpedance. Lymphatic Research and Biology, 10.1089/lrb.2019.001.
https://www.lipedema.org/research-impact


